When does hand-foot syndrome usually appear?
Hand-foot syndrome usually appears in the first 2-3 months of treatment. But, it can appear in the first month especially when using targeted agent. It often begins as redness in the hands and feet, more common to start at the palms first. The redness is usually a patch over the palm, then gradually extends to the whole palms and soles with dry skins and crackings over the joints in the hands and feet.
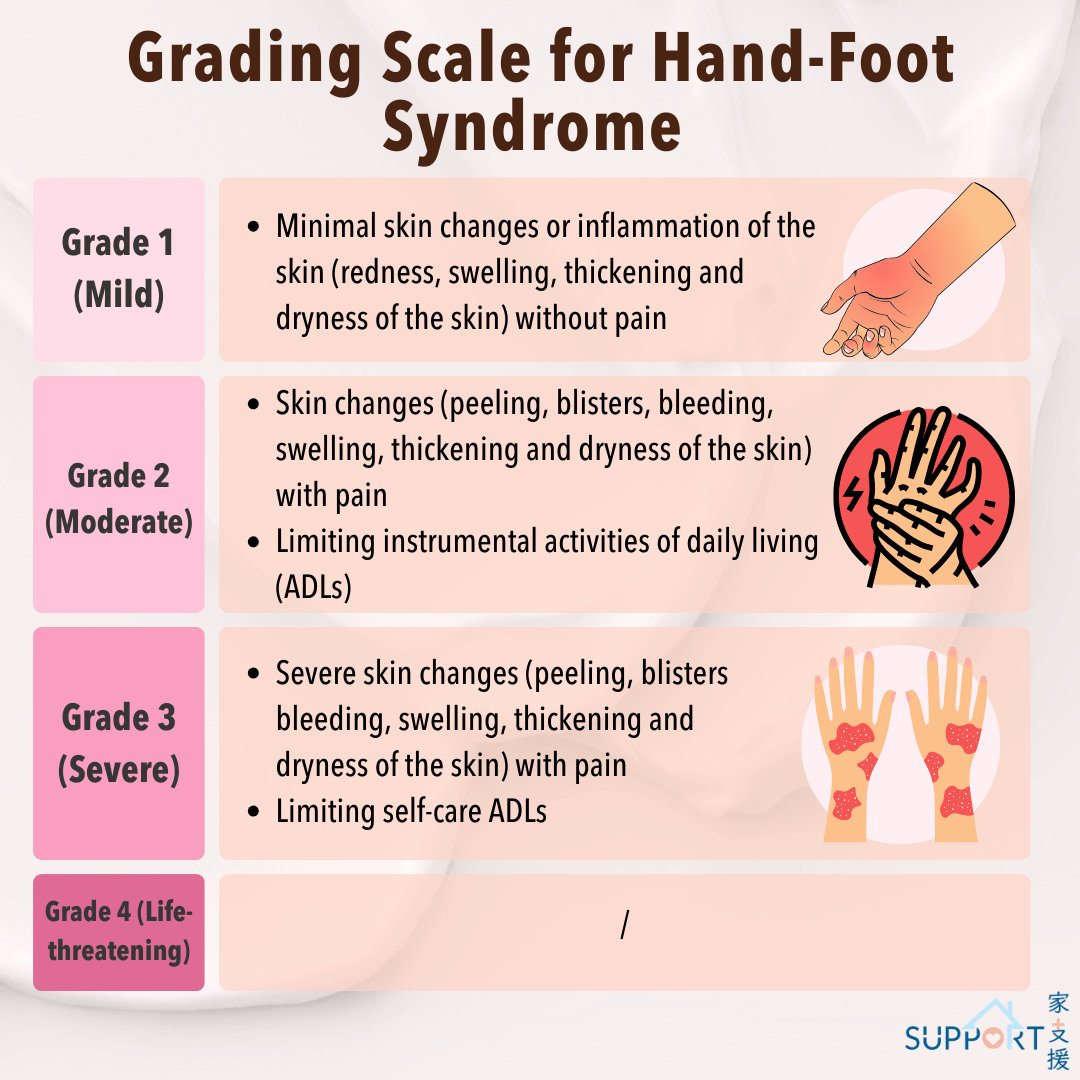
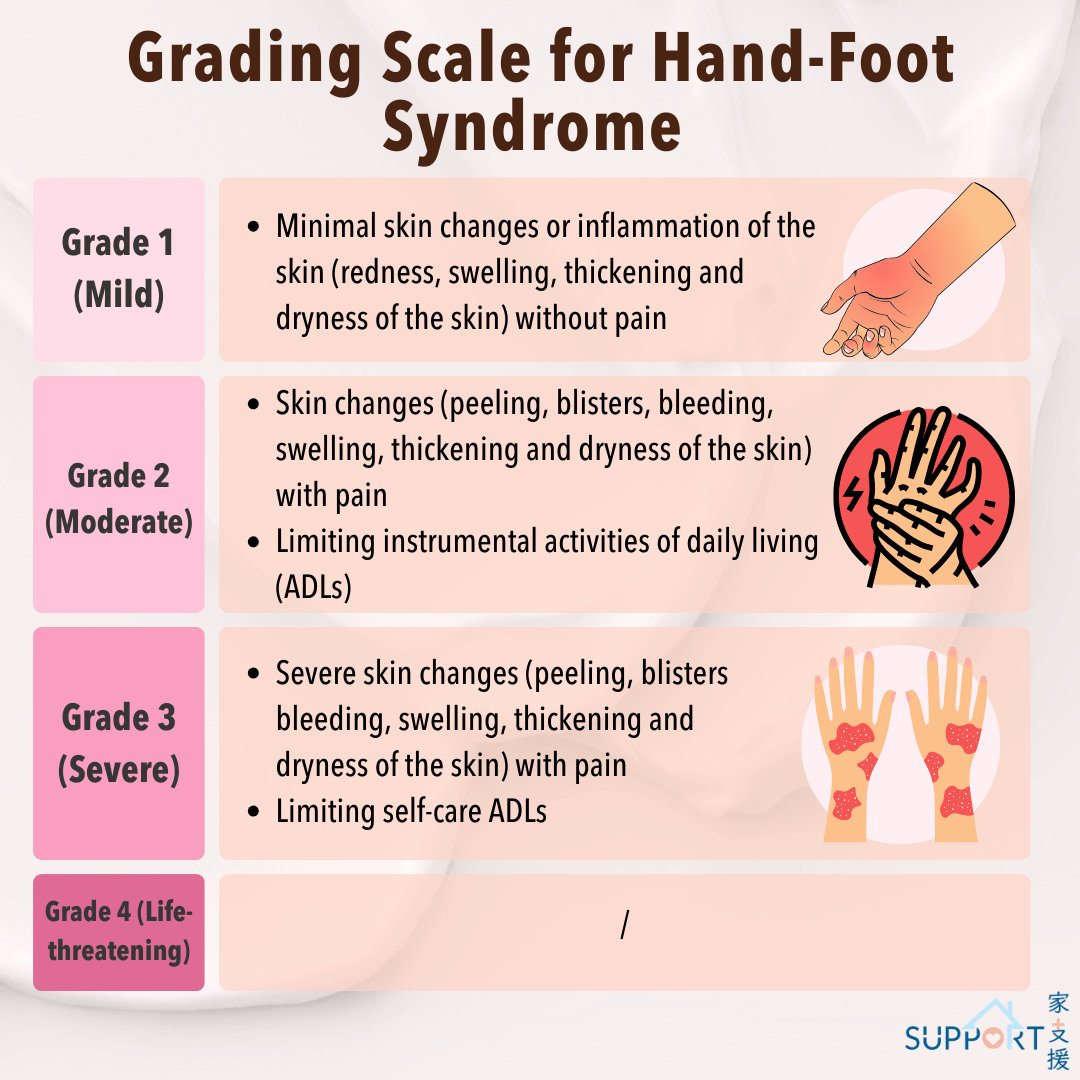
Grading Scale for Hand-Foot Syndrome (NCI CTCAE version 5.0)