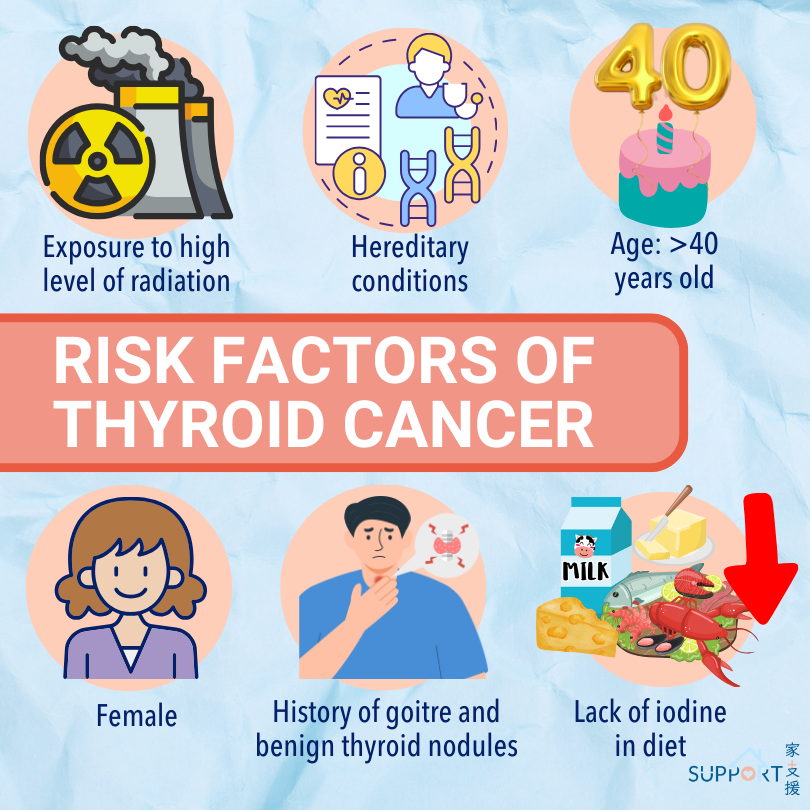
Thyroid cancer was the eighth most common cancer in Hong Kong. In 2023, there were 1,267 new cases of thyroid cancer, accounting for 3.3% of all new cancer cases in Hong Kong, with 278 being males and 989 being females. Women have a much higher chance of getting the cancer than man, and the female to male ratio was about 3.3 to 1. The crude annual incidence rate of cancer per 100,000 Hong Kong population was 17.
Thyroid cancer is usually diagnosed at an early stage. With the advancement of treatments, they are highly curable, which causes its mortality rate to be relatively low in Hong Kong. However, as the cancer develops slowly, there is still a chance of recurrence several years after the initial treatment. Therefore, regular follow-up is recommended.
What is thyroid cancer?
The thyroid is a gland in front of the neck beneath the voice box which shapes like a butterfly. It is an endocrine tissue which is responsible for the production of thyroxine. Thyroxine is needed to keep the body functioning, which affects blood sugar level, heartbeat and kidney function. Situated behind the thyroid gland are parathyroid glands which secrete parathyroid hormone. Parathyroid hormone helps regulate calcium level in the body.
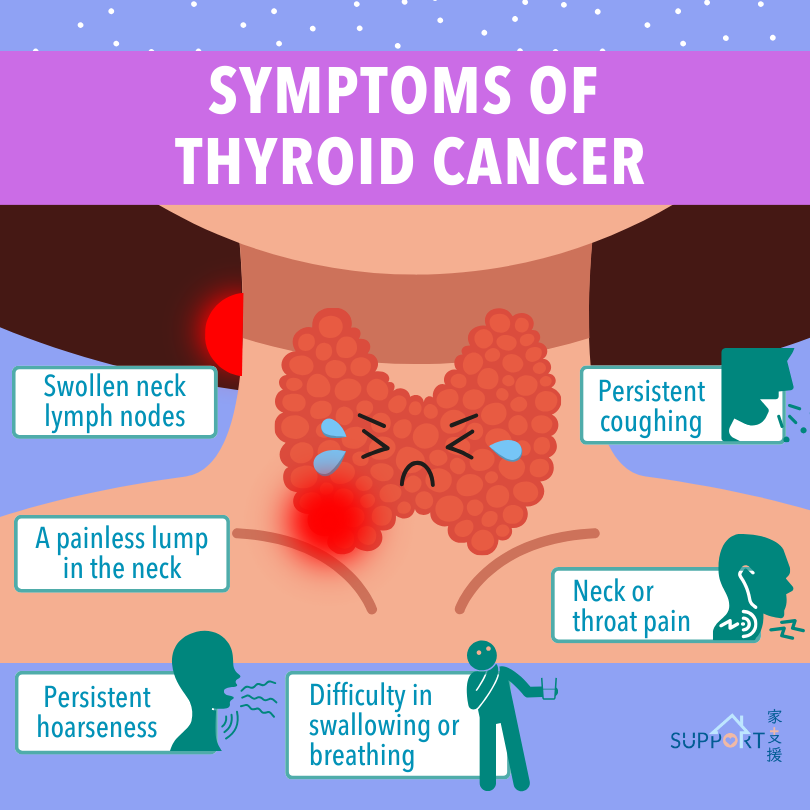
Thyroid cancer is that cancer cells grow abnormally in the thyroid gland and it may spread to the regional lymph nodes or other sites, e.g. lung and bone.