Firstly, euthanasia is defined as “direct intentional killing of a person as part of the medical care being offered”, which is in essence killing a patient to end their suffering. The act can be considered as criminal and is ethically controversial.
Same as most places in the world, Hong Kong does not legally permit euthanasia and it violates the professional ethics of healthcare workers.
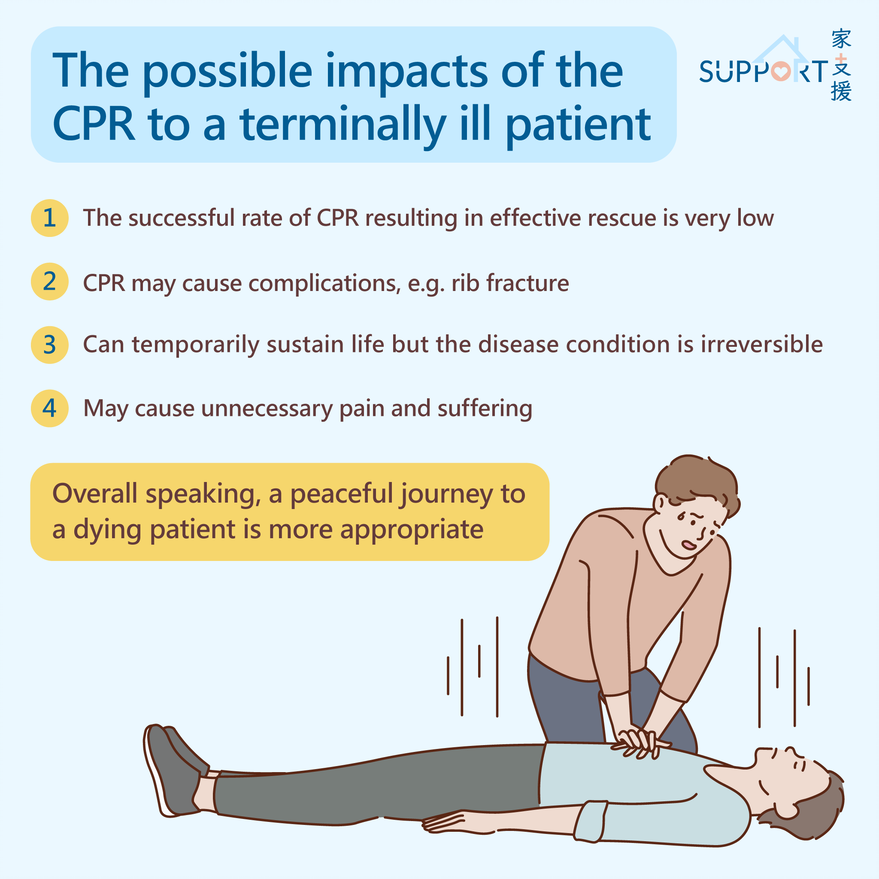
However, the patient has the right to refuse unwanted treatment, including LST such as Cardiopulmonary Resuscitation (CPR). A healthcare professional who provides treatment against the patient’s will may be liable to legal action for battery or assault.
Withholding such treatment in this case is an act of respecting the patient’s wish and ensuring them a peaceful death. This is not tantamount to performing euthanasia.
Withholding or withdrawing futile treatment for a patient is not performing euthanasia as the treatment is not in the best interests of the patient. Administering futile LST on a dying patient would only inflict more suffering. What the patient needs in the final days is not futile treatment, but end-of-life care and a peaceful death.