Types of treatments
Cervical cancer is often treatable. The treatment depends on:
- Size and type of cancer
- Site of the cancer and extent of spread
- Your general health
- Whether you want to have children
1. Surgery
- Surgery is often the main treatment for early cervical cancer.
- Surgery should be performed by an obstetrician-gynaecologist specialising in oncology. It can be open surgery or laparoscopic or robotic-assisted.
- There are different types of surgeries for cervical cancer:
- Conization/ Loop electrosurgical excision procdeure (LEEP): Just for removal of cervical cancer that can only be seen with a microscope, called microinvasive cancer
- Radical trachelectomy: Mainly for young patients who want to preserve fertility. This procedure involves removal of the whole cervix but keeping the uterus intact.
- Hysterectomy, bilateral salpingo-oophorectomy: This procedure removes the uterus, cervix, upper vagina, both fallopian tubes and ovaries. Extensive lymph node dissection is also performed.
- Possible complications:
- Bleeding or haematocele (collection of blood) of vagina
- Wound infection
- Difficulty in urination, usually recover after a period of time
- Oedema (fluid retention causing swelling of the affected area) of lower limbs, mild numbness of the thighs
- Lymph accumulation in the pelvic cavity causing lymphocele (a large, cystic mass filled with lymphatic fluid) and subsequently get infection
- Unable to be pregnant
- (Rare) Damage of the bladder, ureter and rectum during operation
- (Rare) Damage of the major blood vessels during operation, causing severe bleeding or even death
2. Radiotherapy
- Radiotherapy uses high-energy x-rays to destroy cancer cells. Radiotherapy can be given after surgery to reduce recurrence, given alone or concurrently with chemotherapy to kill the tumour.
- The details and frequency of radiotherapy mainly depend on the pathological type of the cancer, the stage of the cancer, the age and health of the patient.
- Clinical applications of radiation therapy for cervical cancer include:
- Main treatment, with or without concurrent chemotherapy (usually for Stage IB to 4A cervical cancer)
- Adjuvant radiotherapy with or without concurrent chemotherapy after surgical resection (to reduce the chance of local recurrence)
- Radiotherapy for cervical cancer can be divided into:
- External beam radiotherapy
- Brachytherapy (internal radiotherapy)
- If radiotherapy is the main treatment for killing the cancer, you will usually receive 4-5 weeks of external beam radiotherapy then 3-4 times of brachytherapy afterwards.
A. External beam radiotherapy
External beam radiotherapy is the use of linear accelerator to send high-energy rays to the tumour and whole pelvis to eradicate the tumour.
Procedure:
- You will have a CT for radiotherapy planning.
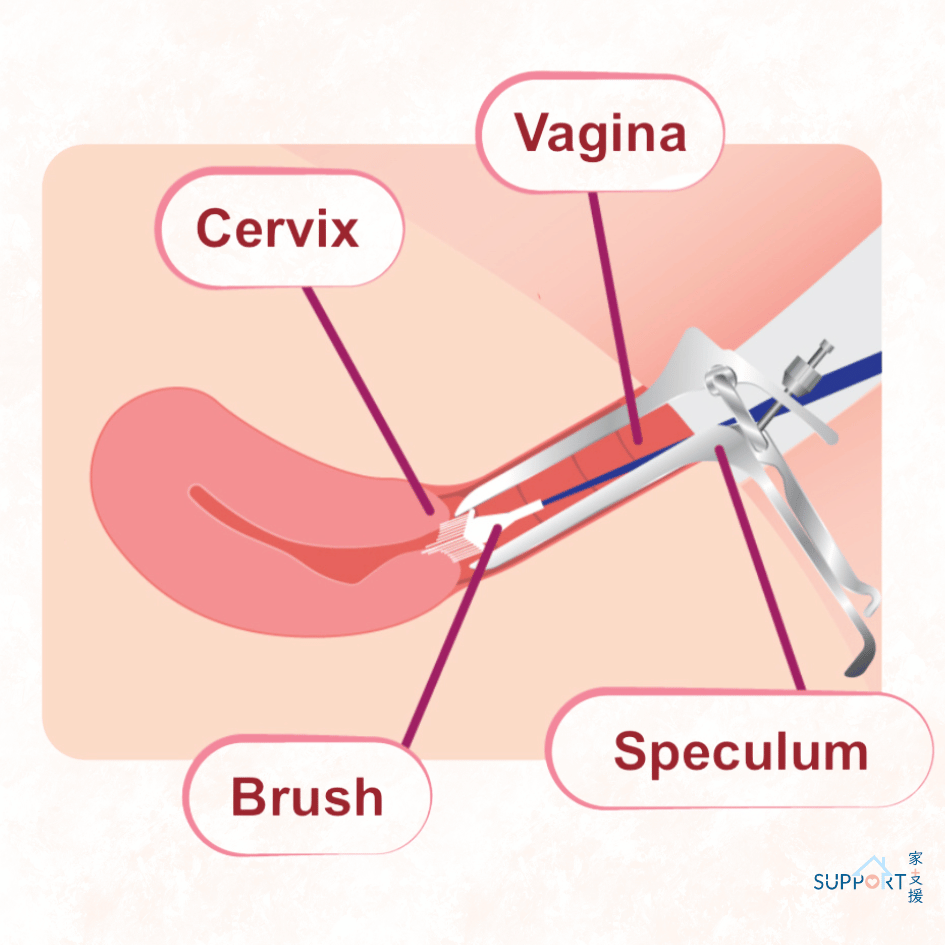
- Before the CT scan, you will need to drink a few cups of water so that you have a full bladder. The radiation therapist will put a little marker outside the vagina to help assessing the radiation field.
- After the planning CT, your oncologist will decide the final details of your radiotherapy plan.
- A common course of treatment is Monday to Friday, with one treatment per day, for a total duration of about 4 to 7 weeks.
- When radiotherapy is used as the main treatment for cervical cancer, it is usually combined with chemotherapy, called cisplatin. The chemotherapy is given weekly to increase the effectiveness of radiotherapy.
- During treatment, you will be asked to drink a certain amount of water so that your bladder is full (similar to the procedure before planning CT). You will also lie in the same position on the couch as when you had your planning CT.
- The whole radiotherapy will last for 10 to 20 minutes.
Possible side effects of external beam radiotherapy
Short-term side effects:
- Fatigue
- Sore and red skin in the treatment area
- Bladder irritation and pain
- Stomach discomfort
- Diarrhoea or loose stool
- Nausea and vomiting
Long-term side effects:
- Skin over the treatment area becomes tighter and less elastic
- Vaginal dryness and getting narrower
- Swelling of the legs
- Easy fullness of the bladder
- Rarely cause bowel obstruction
B. Brachytherapy (internal radiotherapy)
Brachytherapy or internal radiotherapy means putting a source of radiation in or near the cancer. This treatment gives a high dose of radiation to the cervix but a much lower dose to the surrounding organs.
Procedure
- The entire treatment is conducted in the operating room under general anaesthesia or spinal anaesthesia.
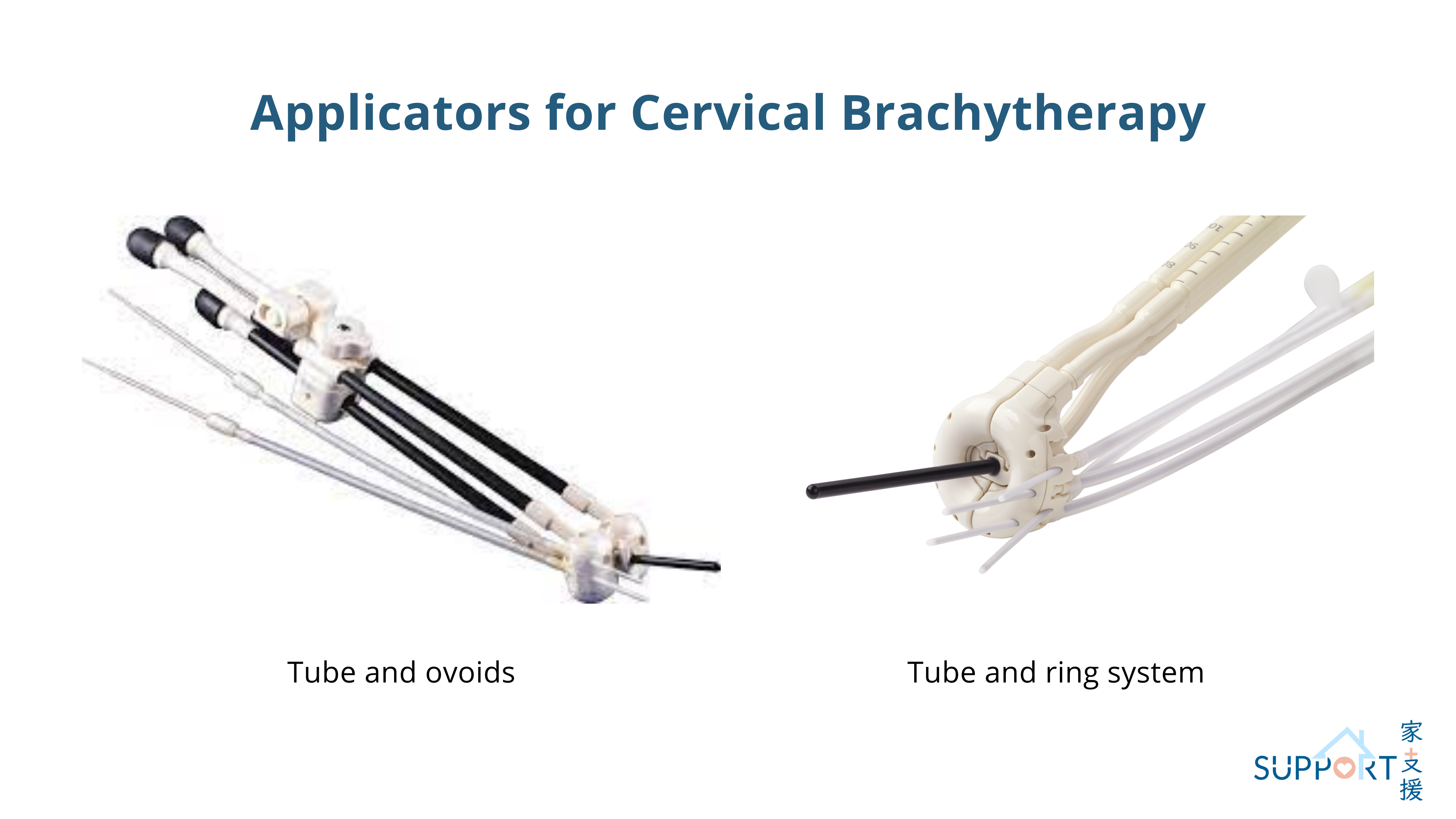
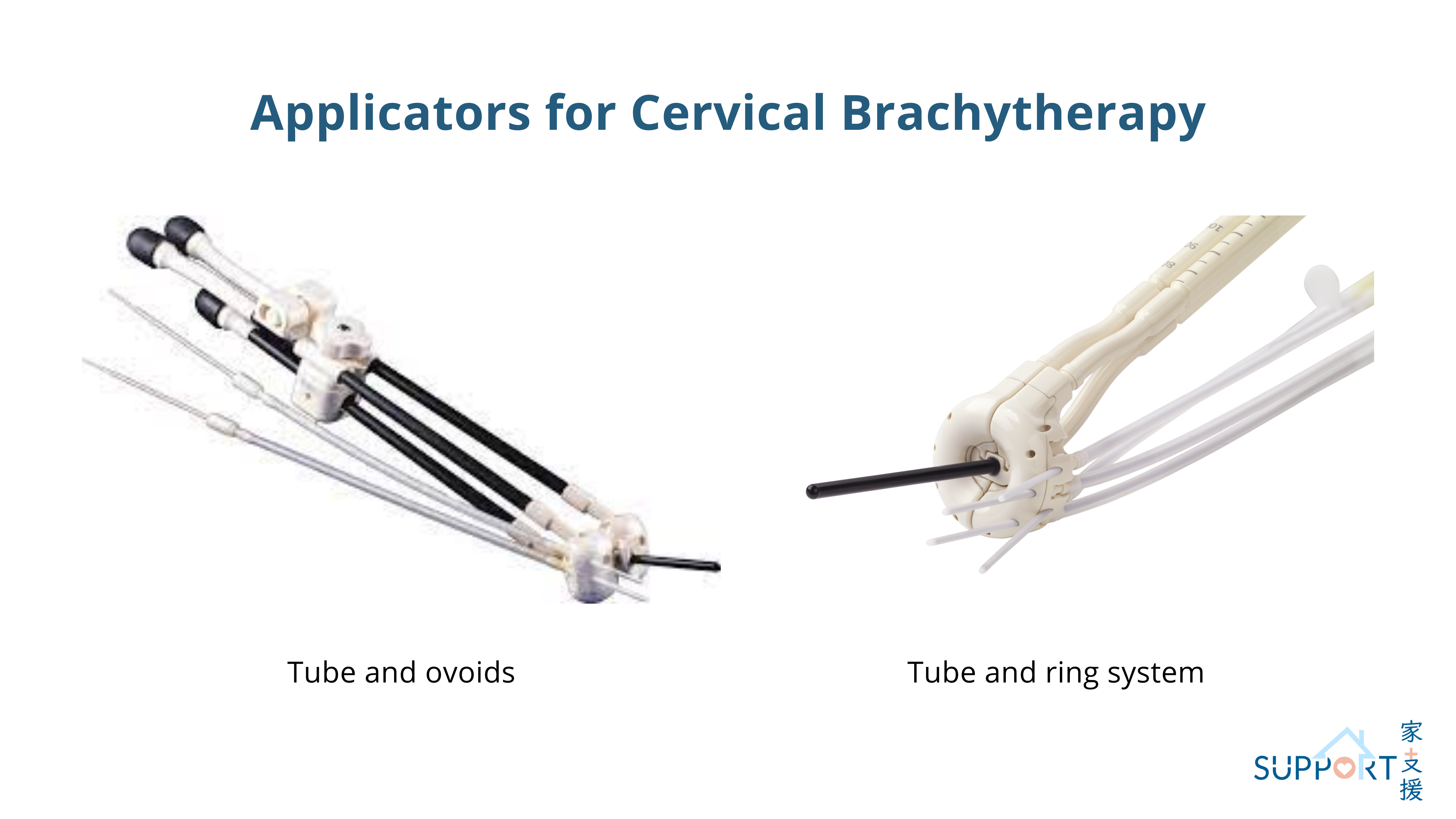
- The doctor will put the applicators into the vagina and cervix. The applicators are made of a small metal tube, and two small round ovoids or two half-rings. Needles may also be inserted if the tumour is very bulky.
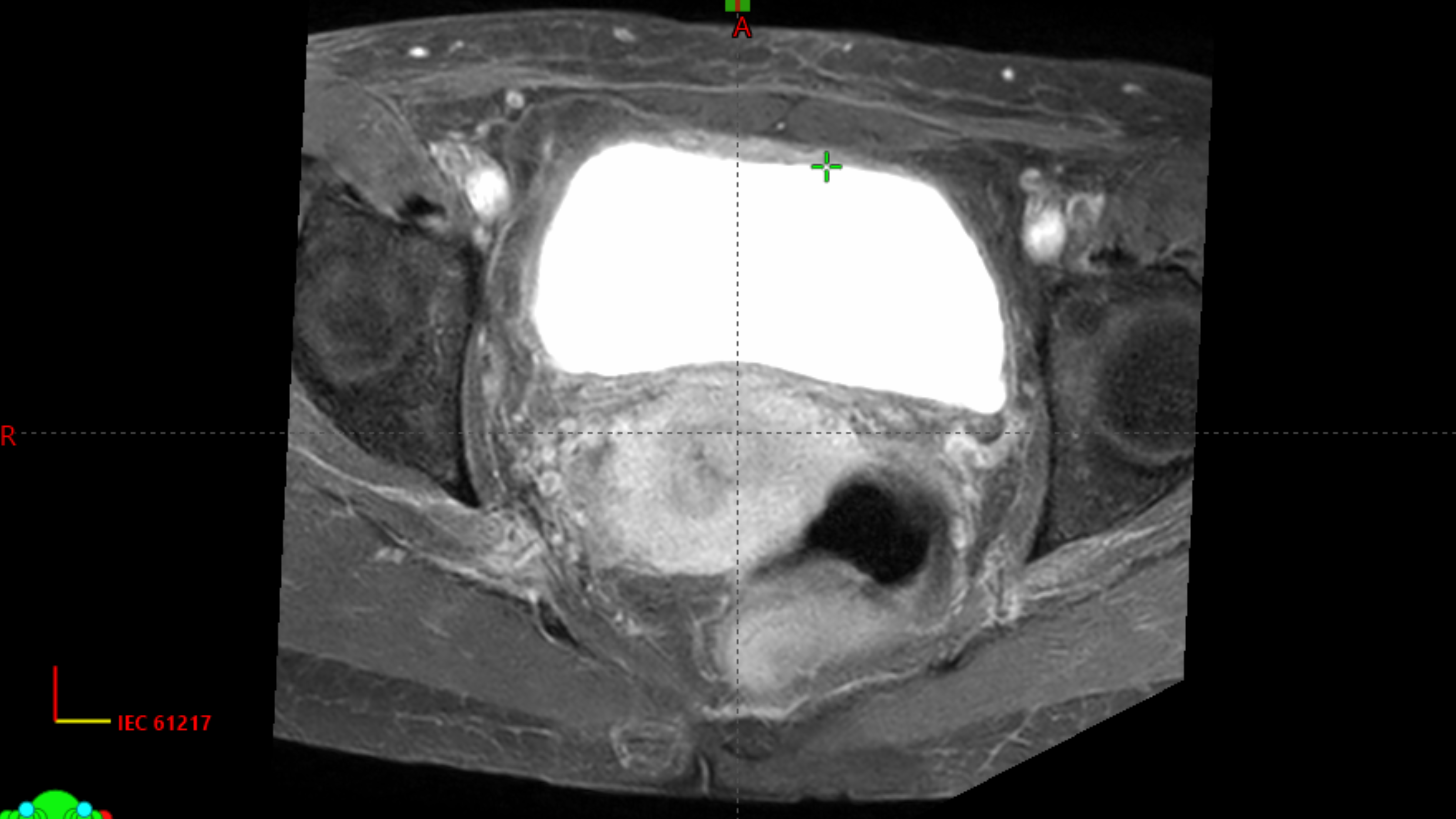
- After the applicators are in place, a CT or MRI will be performed to locate the tumour. The treatment team will produce the brachytherapy plan.
- Once the plan is ready, the radiation therapist will connect the applicators with the afterloading machine.
- After treatment, the applicators will be removed.
- Patient usually needs to undergo 3 to 4 times of treatment in 2-3 weeks. The whole process including brachytherapy planning lasts around 2 to 3 hours while the brachytherapy treatment itself lasts for 15 to 25 minutes.
Side effects of brachytherapy:
- Risks from anaesthesia
- Urinary tract infection
- Vaginal bleeding
- Fatigue
- Diarrhoea
- Bladder irritation or pain
- Narrowing and dryness of the vagina
- Less common: perforation of the uterus, vaginal bleeding
3. Chemotherapy
Anticancer drugs destroy and disrupt the growth and division of cancer cells, which can shrink the tumour. Chemotherapy is usually given together with radiotherapy as the main stream of treatment in patients with Stage IB to 4A cervical cancer.
Procedure:
- The most common chemotherapy for cervical cancer is cisplatin. If your renal function is not satisfactory, your doctor may switch the regimen to carboplatin or epirubicin.
- You will have chemotherapy once a week over the 4-5 weeks of external beam radiotherapy.
- You will have blood tests before chemotherapy to make sure your cell counts are fit.
- The chemotherapy will be given through a drip (infusion) into one of your veins.
Possible side effects:
- Loss of appetite
- Nausea / vomiting
- Diarrhoea
- Fatigue
- Mouth sores
- Increased risk of infection
- Renal impairment
- Neuropathy: numbness of hands and feet
4. Immunotherapy
- Immune-checkpoint inhibitor, Pembrolizumab (Keytruda), can be used in combination with platinum-based chemotherapy and external beam radiation therapy in locally advanced cervical cancer patients. It is a monoclonal antibody that targets and blocks PD-1, a specific protein on the surface of immune cells (T-cells). Blocking PD-1 triggers the T-cells to identify the cancer cells and initiate an attack to kill the cancer cell.
- Administration: intravenous (IV) infusion
- Concurrent with chemoradiotherapy every 3 weeks for 5 cycles, then every 6 cycles for 15 cycles
- Common side effects:
- Fatigue and weakness
- Nausea
- Skin changes
- Loss of appetite
- Hypothyroidism
- Diarrhoea
- Fever
- Adrenal insufficiency
- Severe side effects (Incidence is usually low, <5%)
- Impaired renal function
- Impaired liver function
- Severe skin reaction
- Severe diarrhoea
- Neuropathy
- Inflammation of the lung
- Inflammation of the eyes