According to the 2022 statistics data released by Hong Kong Cancer registry, uterine cancer ranked the fourth most common female cancer in Hong Kong, accounting for 6.6% of all new female cancer cases. There were 1,188 new cases of uterine cancer in 2022. On average, one out of 56 females were diagnosed with uterine cancer. The median age at diagnosis was 57.5 years old.
Uterine cancer was the eleventh leading cause of female cancer deaths in Hong Kong. In 2022, it claimed 109 deaths, accounting for 1.7% of all cancer deaths.
What is uterine cancer?
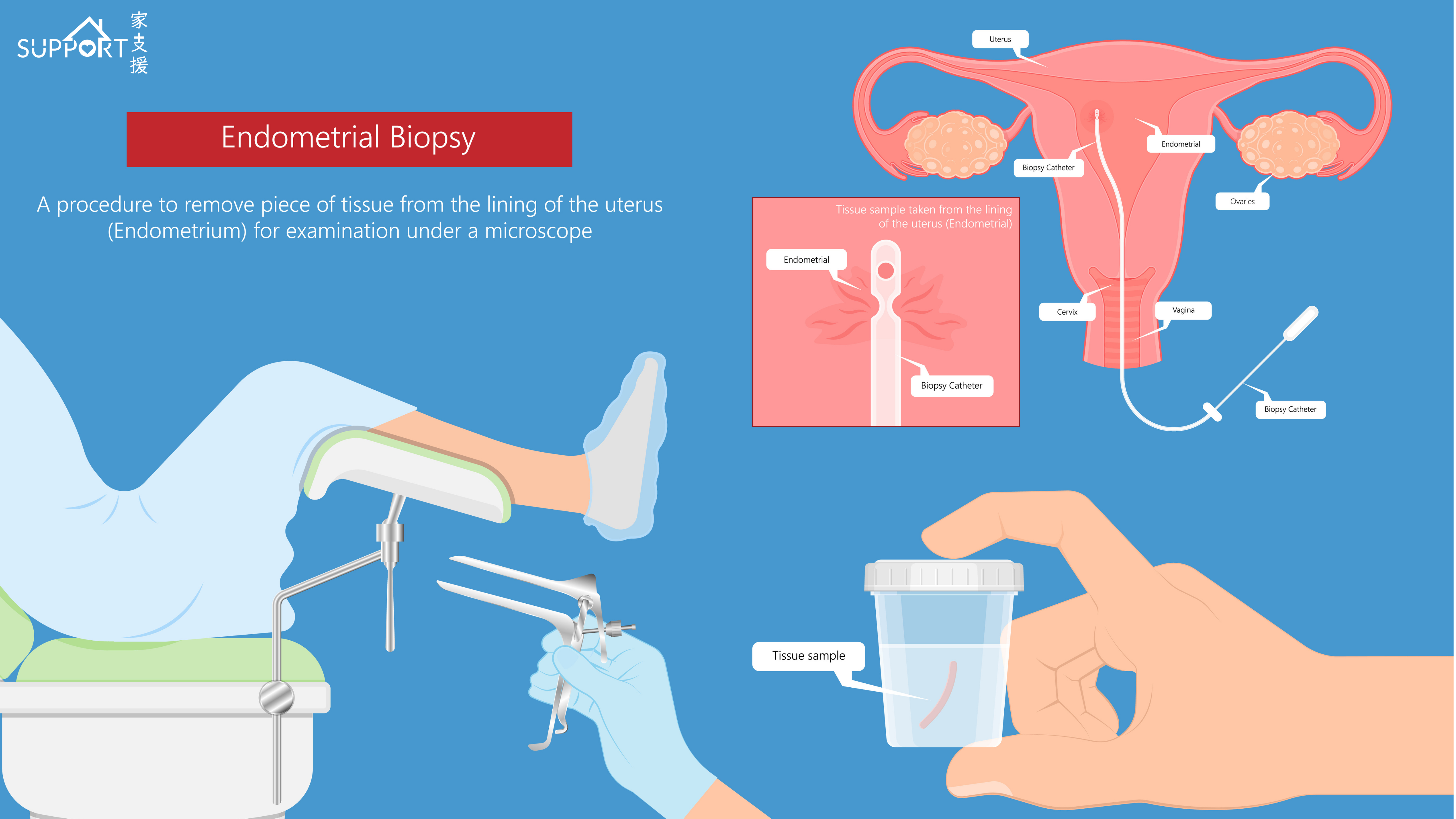
The uterus is part of the female reproductive system, located in the pelvic region in the lower abdomen. The uterus is connected to left and right ovaries by 2 oviducts, and the lower part of uterus is connected to the cervix and vagina.
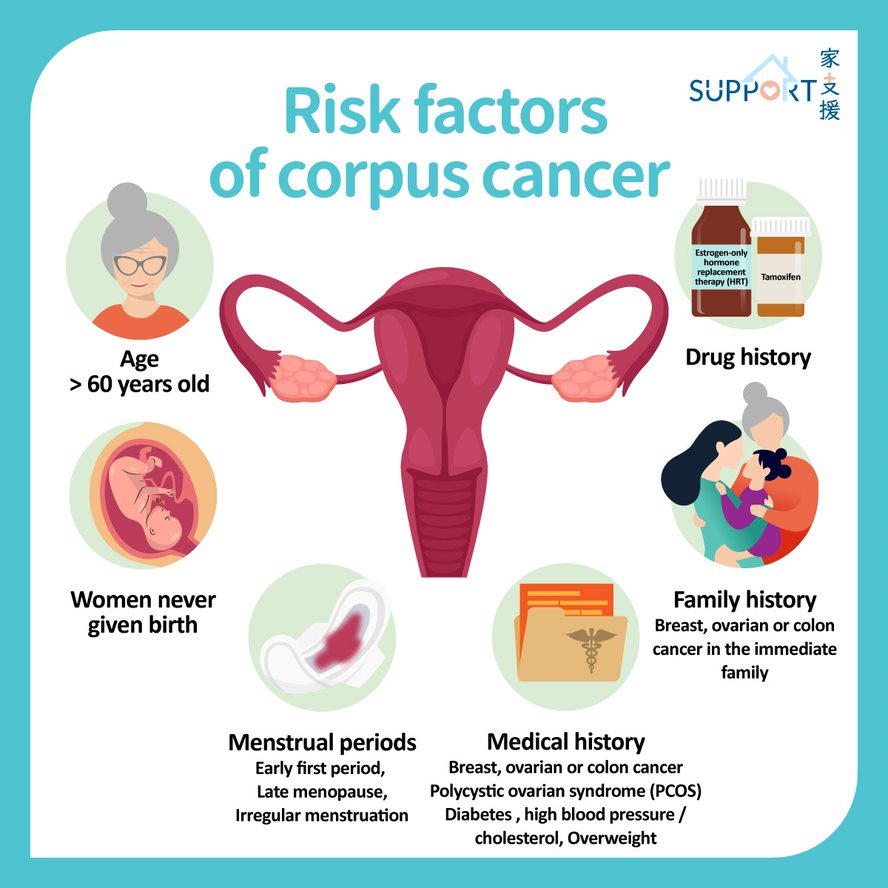
It is composed of mainly three layers: the endometrium (inner layer), myometrium (muscular middle layer), and perimetrium (outer layer). The endometrium is composed of numerous capillaries (small blood vessels). Its main function is to provide an appropriate environment for embryo implantation. Female hormones secreted by the ovaries (estrogen & progesterone) are key components towards the normal growth of endometrium. An abnormal secretion is linked with an increased risk in uterine cancer.
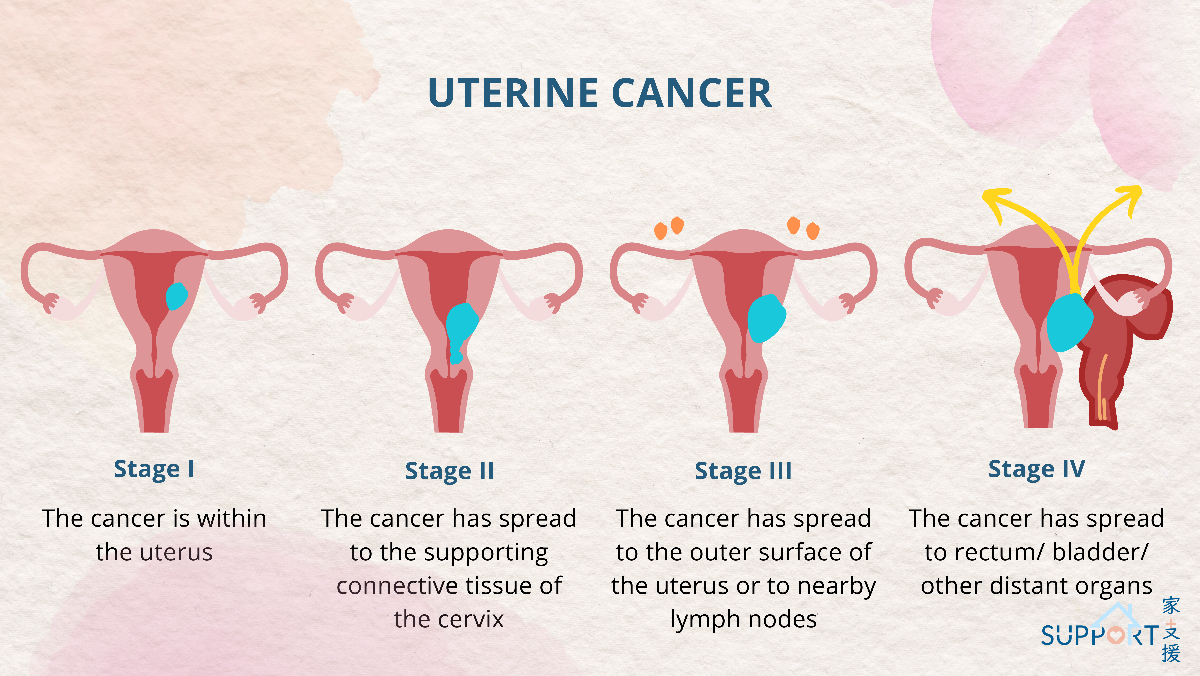
Uterine cancer is a cancer growing from the endometrium. In mid to late stage, cancerous cells will spread to structures near the uterus. It may also spread through lymph and bloodstream to other organs like liver and bones.