What is my responsibility as a carer during my patient’s last stages?
As a carer, the most important thing to do is to accompany the patient under care during the final, and often the most difficult phase of their life.
The things that must be done during the patient’s last few days of life depending on where they are. If they have chosen to die at home, one may need to shoulder much more responsibilities, as these could include administering medications, keeping the care environment clean and comfortable, and most importantly, calling the patient’s healthcare team or emergency services if necessary.
Regardless of where this care takes place, the healthcare team will provide the best support to both the carer and patient during the whole process.
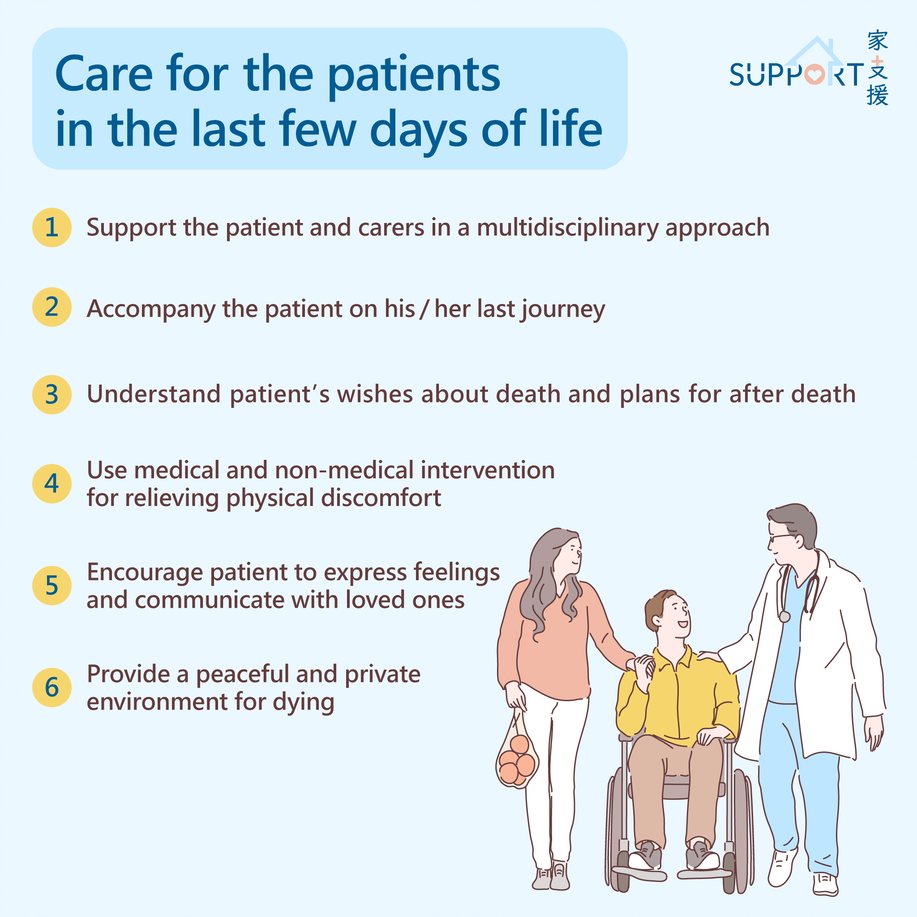
What are the main goals of care during the patient’s last few days?
- Making sure that the patient is physically, psychologically and spiritually comfortable
- Guaranteeing that the process is dignified and peaceful
- Supporting the patient and close family members. Take care to ensure most, if not all, memories of the entire process should be as positive as possible.
- Getting to know as much as one can about the patient’s wishes about death and dying, as well as plans for after death.
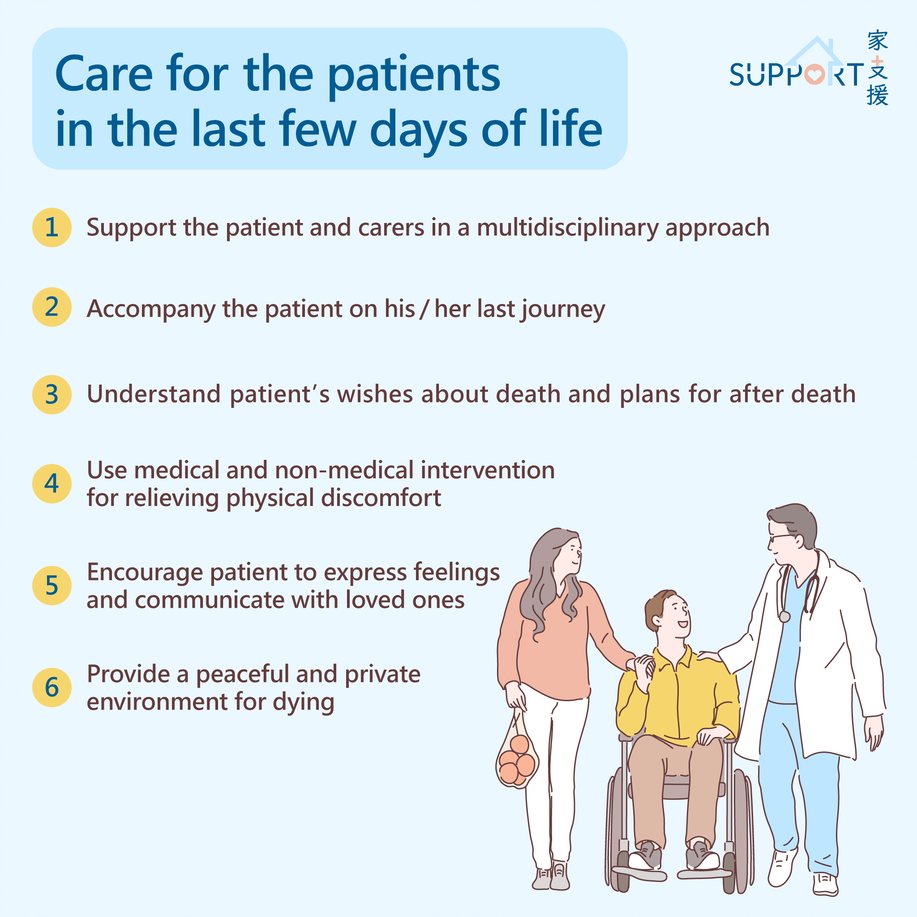
How will doctors help the carer and patient?
- The doctor will give professional advice and suggestions. Listen and remember them as clearly as possible.
- The doctor may ask you questions about the preferred location of death, any support at home, home environment, issues about cremation, financial, and other ‘unfinished business’.
- One may be encouraged to participate in the physical care of the patient.
- The doctor will review your patient’s condition and medication history. They will prescribe medications generally to relieve any discomfort. These may include painkillers, anxiolytics (medications to relieve anxiety), and anti-convulsants (medications to control convulsions). If the patient cannot swallow, the medications may be given intravenously (through the veins) or subcutaneously (through the skin).
Is the patient’s doctor in charge the only one involved in end-of-life care?
- Rest assured - an entire palliative care team will support the patient and their family in a multidisciplinary approach. The team includes key members such as palliative care specialists, palliative care nurses, psychologists, social workers, pharmacists and chaplains if your patient is religious.
- The doctor may refer the patient to specialist in the palliative team when distressing symptoms occur and become difficult to control, or when there is severe emotional distress with the patient’s conditions.
How will the palliative care team assess patients’ needs?
- The team will address both the patient’s and your (as a carer) needs and concerns.
- Physical needs
- Common problems including pain, shortness of breath, nausea, oral problems, sleep disturbances, weakness, confusion, the burden of taking medication and pressure sores.
- Both medical and non-medical intervention could be ways to manage the patient’s discomfort. Examples could include using a pressure-relieving mattress to alleviate pressure sores and reduce the need for frequent turning, and medications to relieve noisy breathing – as well as using moisturising eyedrops to reduce dryness of the eyes.
- Psychological needs
- The main goals are comfort and peace. The healthcare team will assess the patient’s needs and any distress that is experienced.
- Anxiety and agitation may need to be managed with medications.
- Examples of the patient’s fears – be they associated with symptoms, morphine prescription or the process of dying.
- During their last days, patients are more often concerned about their family than about themselves.
- Spiritual needs
- Spiritual disquiet or pain may be relieved by allowing the expression of feelings and communication with loved ones. Some patients may have particularly strong emotions, particularly of fear, uncertainty and the urge to address unresolved conflicts or guilt.
- If the patient has any religious beliefs or specific tasks to be accomplished, talk to the nurses and the palliative team to see if the carer can continue these without breaking protocol and regulations. The palliative care team may also help the carer facilitate this wherever possible.
- Dignity
- If the patient chooses to die in a hospice or hospital, both single and smaller wards may be offered for the privacy of both you and your patient.
- If they decide to die at home, a bedroom with close relatives beside them would be more than enough to create a peaceful environment.
Will doctors carry out any investigation?
- There is often little need for investigations at the end of your patient’s life. The patient’s healthcare team will perform an investigation only if the results will change any aspects of treatment plans that are in place. An example could be excluding reversible conditions where treatment could make your patient more comfortable.
- Physical examination is often kept to a minimum to avoid unnecessary distress. During these rare occasions, the doctor may only examine any site of potential pain or any relevant area of the body that might be causing discomfort.
Special thanks to Ms. Elkie Yu-Kiu Chan (Class M25), Mr. Alan Tak-Lok Chan (Class M24), medical student of Li Ka Shing Faculty of Medicine, the University of Hong Kong, and Dr. Wendy Wing-Lok Chan, Department of Clinical Oncology, the University of Hong Kong for authoring and editing this article.
Last updated on 1 Nov 2021.