Surgery
- Surgery can quickly relieve any mass effects caused by brain metastases. However, it is only suitable for cases with milder metastases, tumours involving only one side of the brain or tumours on the exterior as extracting tumours from both sides or deep parts of the brain is risky.
- Before surgery, the patient’s general health condition has to be assessed. Older patients or those who are medically ill are not recommended to be under the surgery, as they are higher in risk.
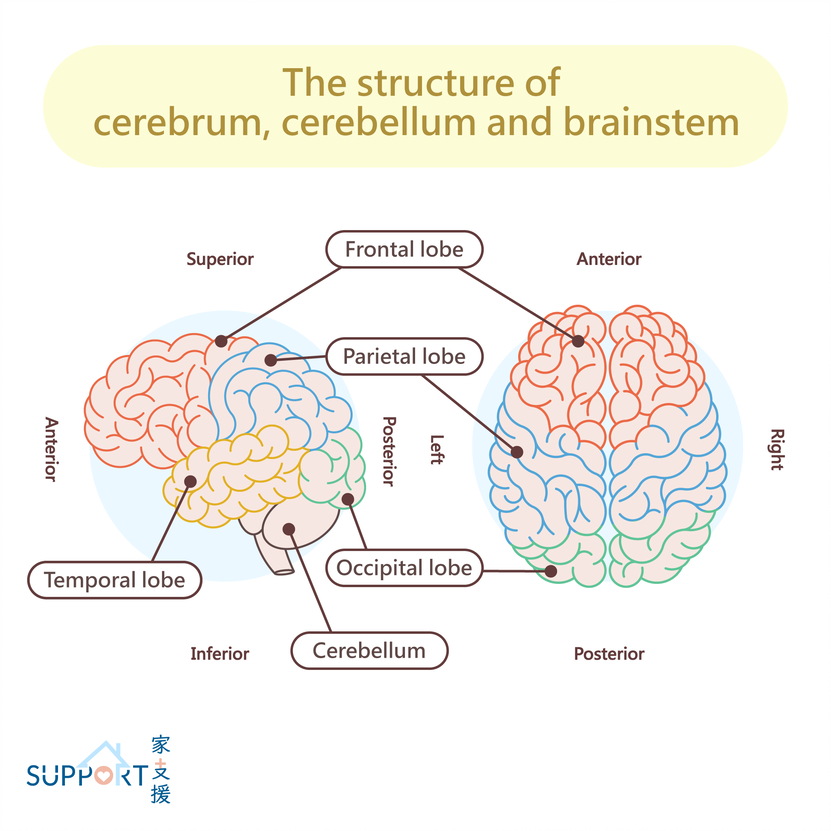
- One major limitation of surgery is the potential irreversible neurological deficit after operation. Some parts of the brain are not operable. For example, resecting tumor at the motor cortex may cause limb paralysis.
Whole Brain Radiotherapy (WBRT)
- Palliative whole brain radiation therapy (WBRT) is commonly used for patients with multiple brain metastasis.
- Side effects of whole brain radiotherapy include fatigue, hair loss, mild headache, nausea and vomiting. These occur usually in the first three months after radiotherapy. Oral steroids are usually prescribed with WBRT to reduce these side effects.
- WBRT may affect the patient’s quality of life and long-term neurocognitive function. However, it is rare to be severely affected.
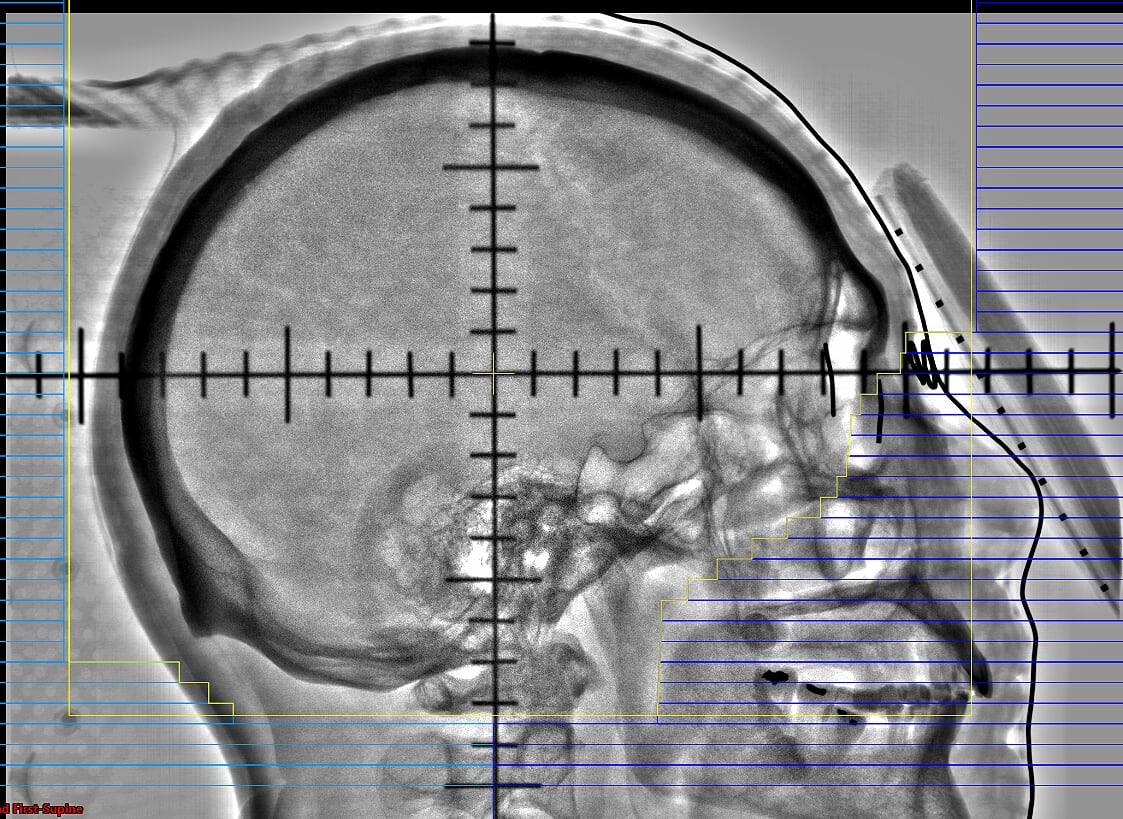
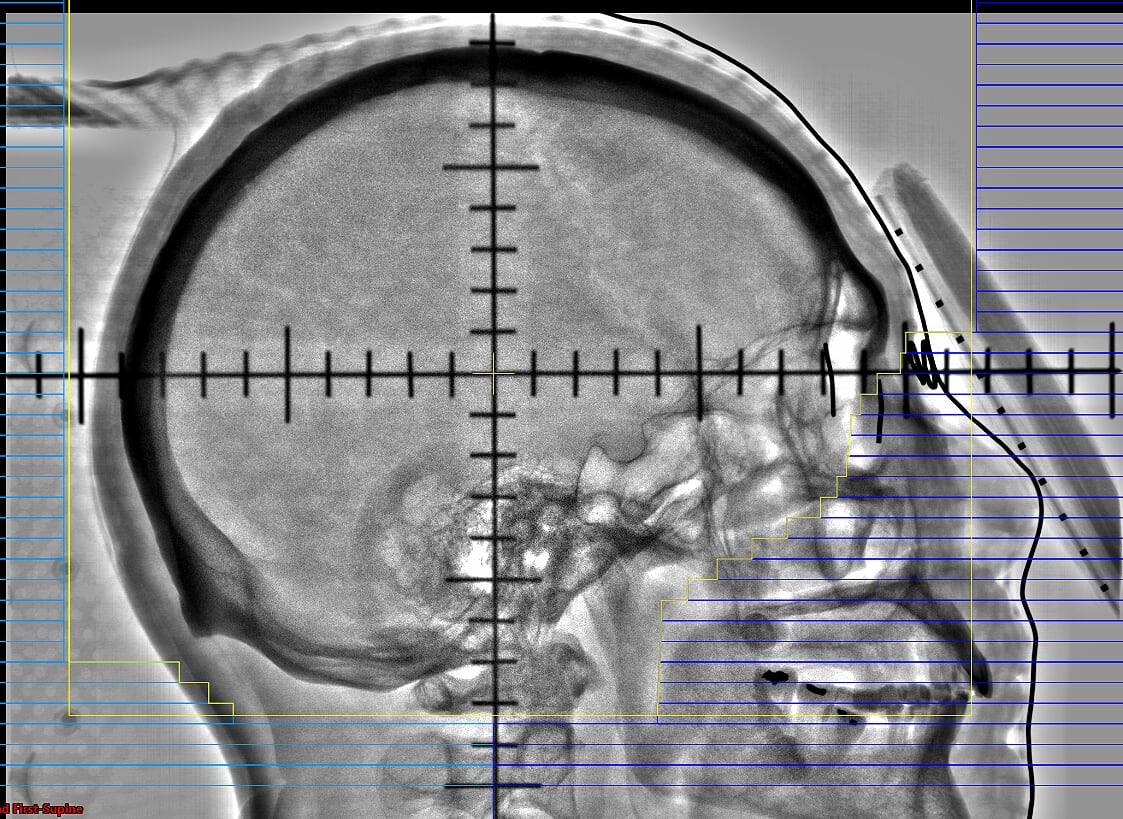
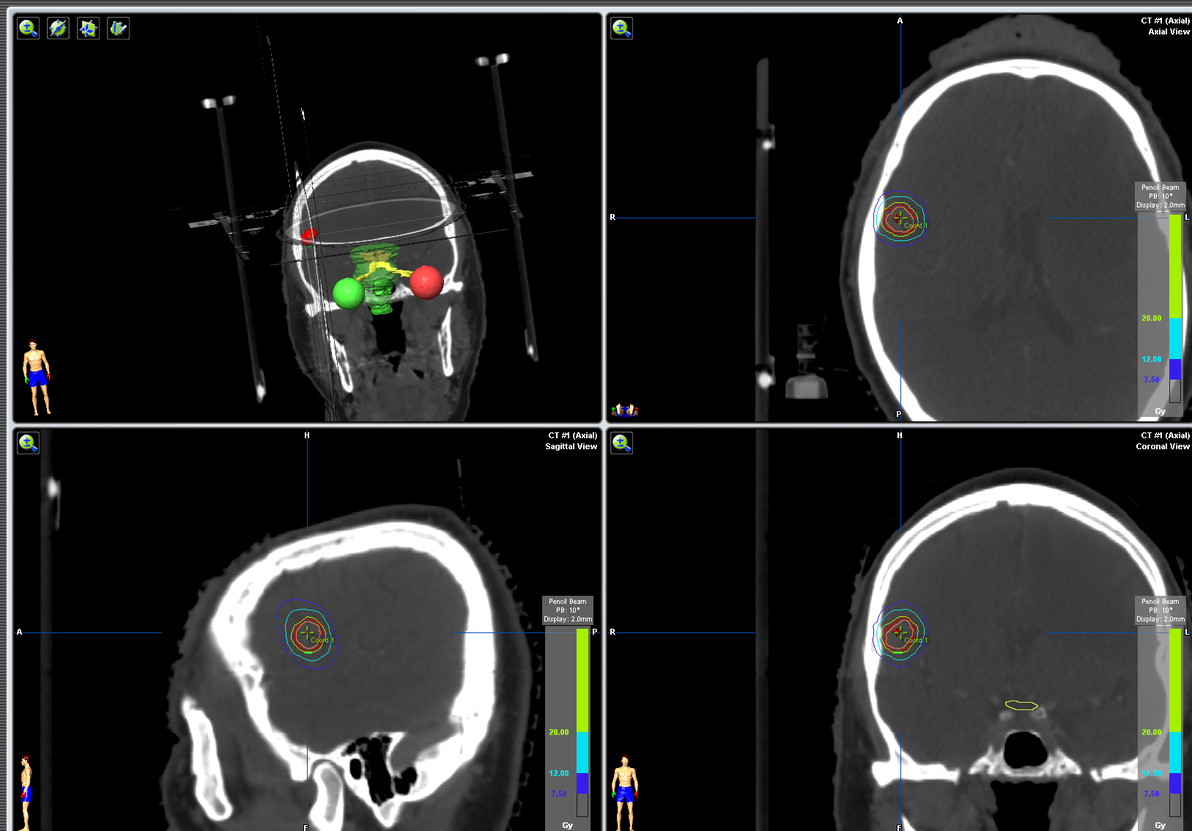
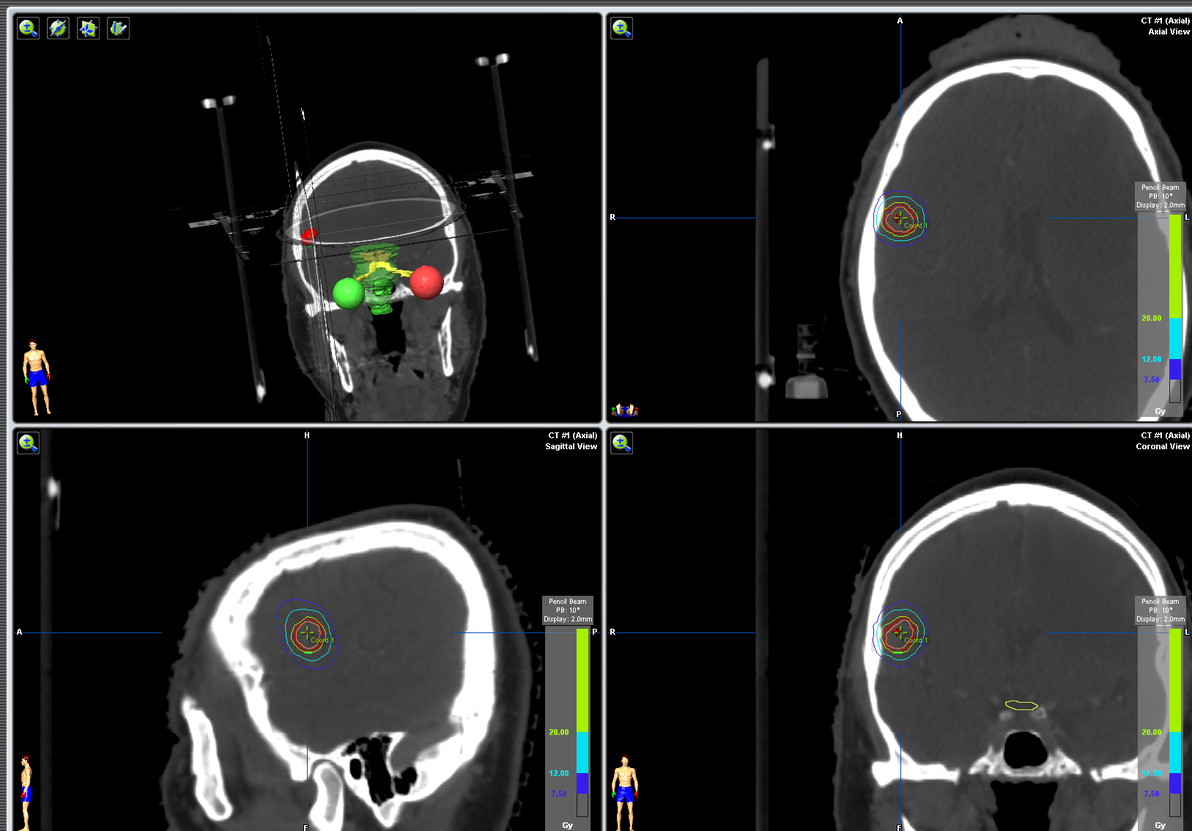
Stereotactic radio-surgery (SRS)
- An effective treatment for localised and small brain metastatic tumours, which are tumours less than 3cm in diameter.
- Compared with open surgery, it can provide similar effects in disease control.
- SRS shrinks tumours over a long time, which is unideal for tumours causing mass effects in the brain.
- With recent advancements in radiotherapy technology, SRS in treating multiple brain metastasis has been more feasible and efficient.
Drug Therapies
- In the past, drug therapies were considered ineffective against brain metastasis due to the “blood brain barrier”.
- Nowadays, with the development of novel anti-cancer systemic treatment, drugs have been designed to improve the drug penetration into the brain. Many targeted therapies and immunotherapies had been proven to be effective for both intracranial and extracranial diseases with similar response rate.
- For example, Osimertinib, a third-generation anti-EGFR targeted agent for metastatic lung cancer, can effectively control brain metastasis with lung primary.
Patients with brain metastasis form a heterogeneous group in terms of their general condition, primary cancer, number and site of occurrence. Each patient will receive a tailored management plan. To provide the best possible treatment, a multi-disciplinary team (MDT) approach can be used. For example, the use of SRS after surgical resection of the brain metastasis in hope of reducing the risk of relapse.