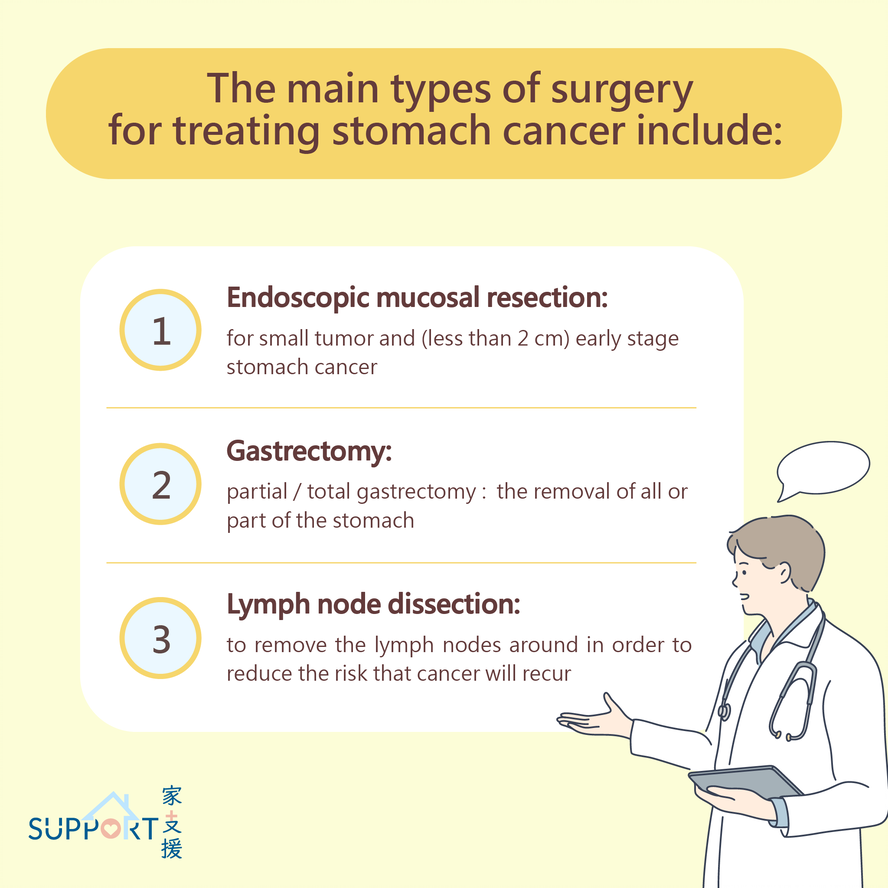
Surgery is often used to treat stomach cancer. The type of surgery depends mainly on the size and location of the tumour. Often during surgery, the lymph nodes close to the stomach are removed at the same time to see if cancer cells have spread into them.
The main types of surgery for treating stomach cancer include:
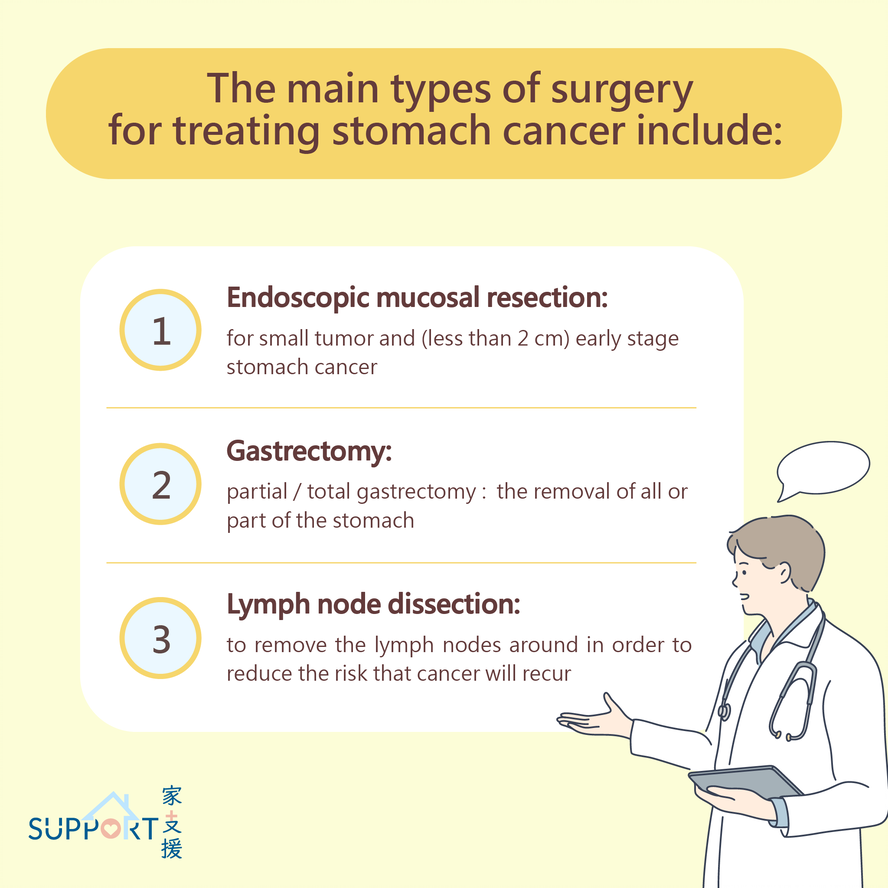
Endoscopic mucosal resection (EMR) or Endoscopic submucosal dissection (ESD)
- Endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) is a very specialised surgery for small (less than 2 cm), early-stage stomach cancer that has not spread beyond the inner lining of the stomach (called the mucosa). ESD is done using an endoscope placed through the mouth, throat and into the stomach. Saline is injected under the tumour to lift it away from the lining for easier extraction.
- The resected tumour is observed under microscope to see if the margin is clear of cancer cells. If there is close margin or residual disease, further surgery is usually required.
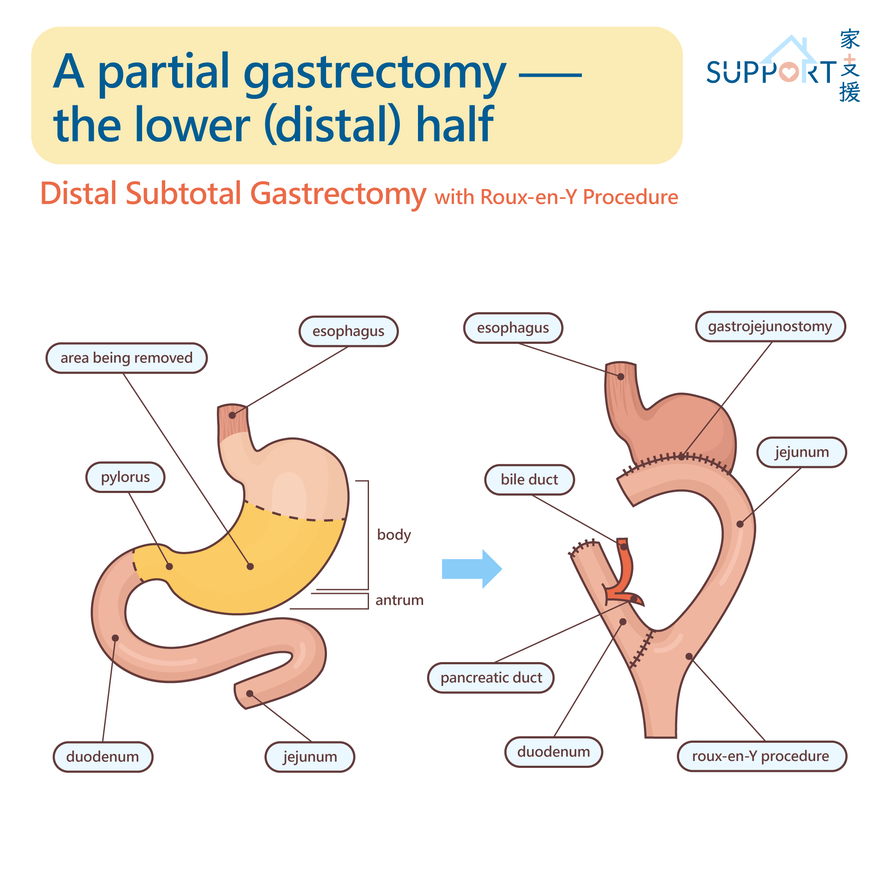
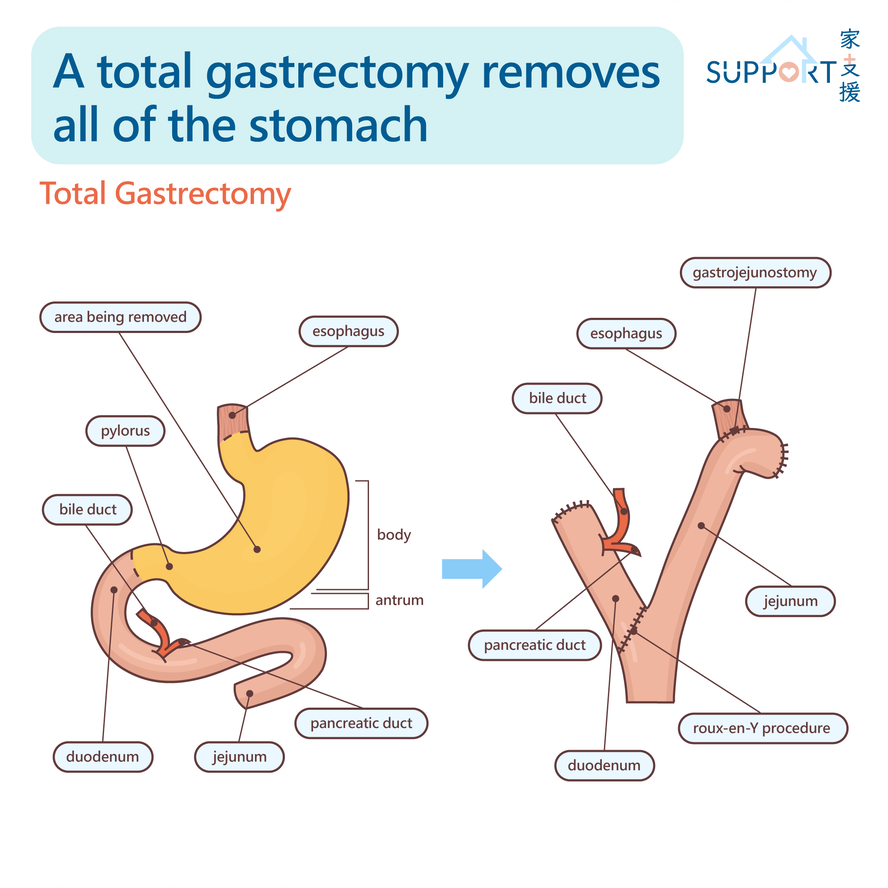
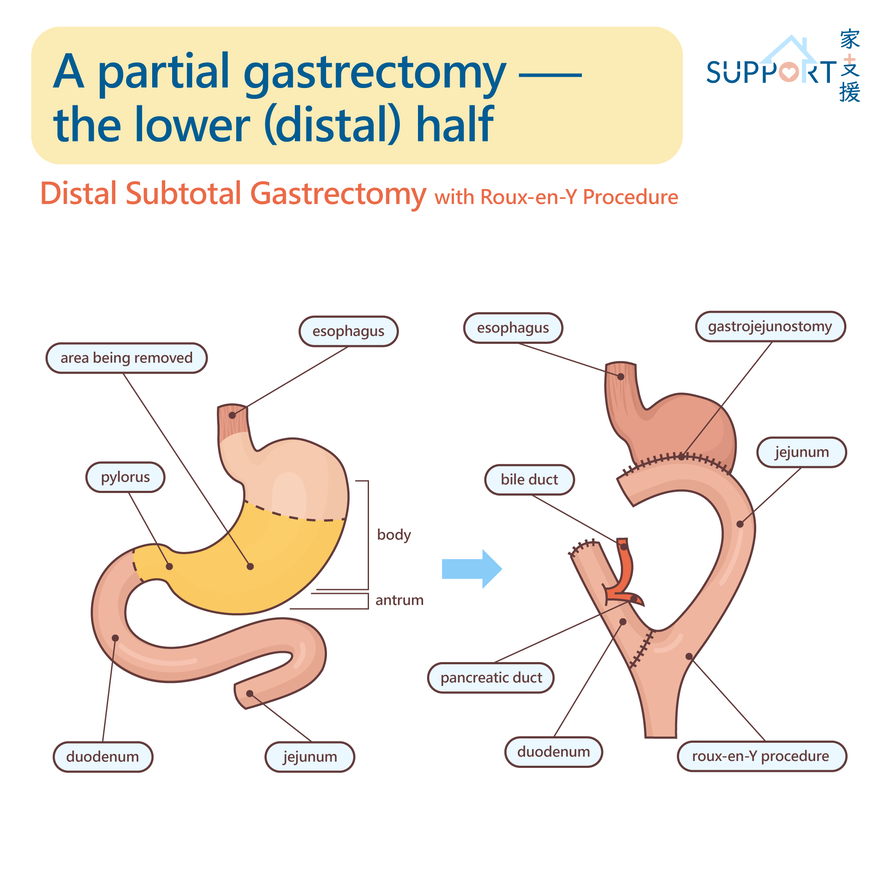
Gastrectomy: partial/ total gastrectomy
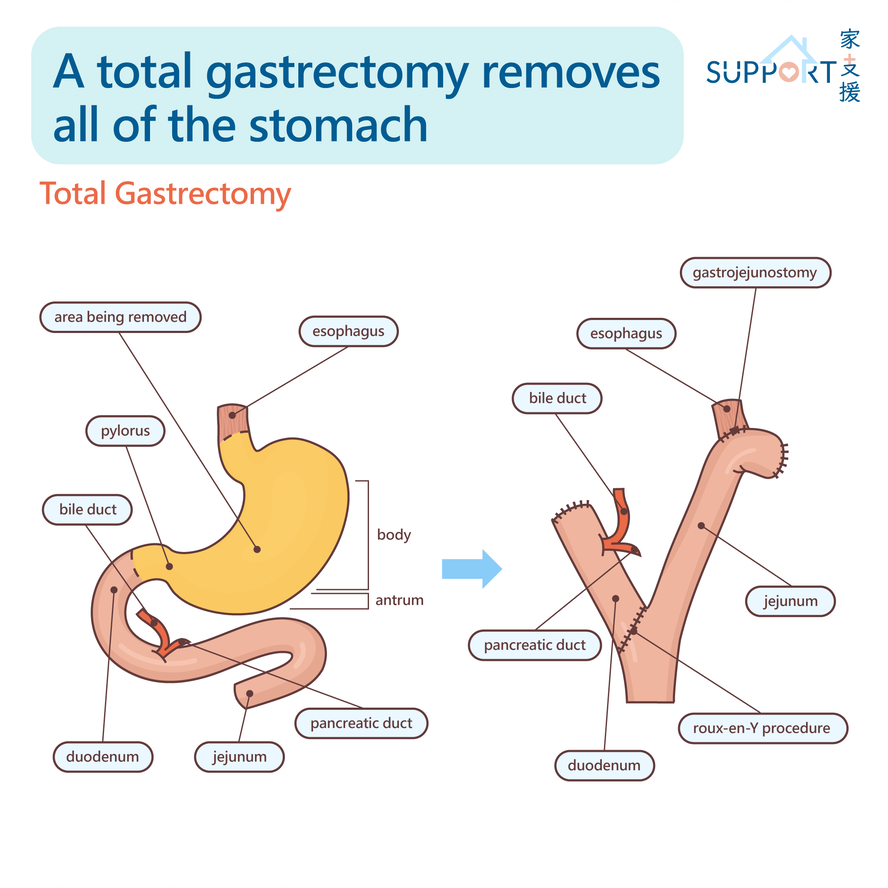
- A gastrectomy is the most common surgery to treat stomach cancer. A gastrectomy is the removal of all or part of the stomach and nearby lymph nodes. The oesophagus is reconnected to the small intestine. Sometimes other organs or structures like the spleen or omentum are also removed during gastrectomy.
- There are different types of gastrectomy. A total gastrectomy removes the whole stomach. A partial gastrectomy removes part of the stomach, either the upper (proximal) or lower (distal) half.
Lymph node dissection
- Since stomach cancer spreads to the surrounding lymph nodes easily, it is important to remove them to lower the chance of recurrence.
- In some East Asian countries, such as China, Japan, and South Korea, surgeons often remove a greater number of lymph nodes (at least 30) along the left gastric, common hepatic, celiac, and splenic arteries.
Neoadjuvant/ Adjuvant treatment
Chemotherapy
Chemotherapy for stomach cancer may be given as a single drug or as a combination of 2 or more drugs. The following are common chemotherapy drugs used before or after stomach surgery:
- Capecitabine and oxaliplatin
- A regimen of two drugs: oral capecitabine and intravenous oxaliplatin. This regimen is usually given every 3 weeks for a total of 8 cycles.
- This regimen may be considered before and after surgery.
- TS-ONE/ S-1
- This is an oral medication that combines three pharmacological compounds:
- Tegafur becomes 5-fluorouracil (5-FU) when metabolized. 5-FU can prevent the growth of cancer cells or result in cancer cell death.
- Gimeracil inhibits 5-FU degradation, and sustains anti-tumour activity.
- Oteracil Potassium reduces digestive side effects such as diarrhoea, while reducing toxicity associated with 5-FU.
- TS-ONE is usually taken twice a day. In one cycle, the patient will continue to take TS-ONE for four weeks then rest for 2 weeks.
- TS-ONE can be combined with docetaxel for Stage III stomach cancer as adjuvant treatment after operation. Adding docetaxel on top of TS-ONE can improve in overall survival and relapse-free survival in patients with Stage III gastric cancer.
-
- 5-FU, leucovorin, oxaliplatin and docetaxel (FLOT)
- Some patients may have received chemotherapy before surgery to reduce the size of the tumour.
- FLOT contains three chemotherapies (5FU, leucovorin, oxaliplatin and docetaxel) can be used. It is given every 2 weeks for four cycles before surgery then another 4 cycles after surgery.
- Common side effects of chemotherapy include:
- Higher risk of infection
- Anaemia
- Malaise/ tiredness
- Sore mouth/ mouth ulcers
- Hair loss
- Early menopause and fertility problems
- Darkening of skin over face, fingers and hands
- Kidney problem
- Hand-foot syndrome

Radiotherapy
Radiation therapy uses high-energy X-rays or particles to disintegrate cancer cells. It is sometimes used together with chemotherapy (e.g. 5-FU) before or after surgery to reduce risks of recurrence.
The high dose radiation for treating stomach cancer may affect the surrounding organs, e.g. liver, bowels, kidneys, spinal cord and heart. Using CT scan for radiotherapy planning can help protect these surrounding organs.
Side effects from radiotherapy include:
- Fatigue/ malaise
- Weight loss
- Mild skin reaction
- Stomach discomfort
- Nausea and vomiting
- Loose bowel movements