Lymphoma is a curable disease. With appropriate treatment, majority of patients will see their condition in remission for many years or even cured. Monoclonal antibodies and chemotherapy are the mainstay of treatment against lymphoma achieving good response rates. Radiotherapy may occasionally be used.
Chemotherapy
- Anti-cancer drugs taken orally as tablets or capsules, or injected into a vein. Examples include:
- ABVD – doxorubicin, bleomycin, vinblastine, and dacarbazine
- AVD – doxorubicin, vinblastine, and dacarbazine
- BV + AVD – brentuximab vedotin + AVD
- Escalated BEACOPP – bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine, and prednisolone
- BrECADD – brentuximab vedotin, etoposide, cyclophosphamide, doxorubicin, dacarbazine, dexamethasone
- VEPEMB – vinblastine, cyclophosphamide, procarbazine, etoposide, mitoxantrone, bleomycin, prednisolone
- ChIVPP – chlorambucil, vinblastine, procarbazine, prednisolone
- CHOP – cyclophosphamide, doxorubicin, vincristine, prednisone
- CVP – cyclophosphamide, vincristine, prednisone
- GCVP – gemcitabine, cyclophosphamide, vincristine, prednisone
- Most chemotherapy drugs given intravenously or orally cannot reach the cerebrospinal fluid (CSF) and tissues around the brain and spinal cord. To treat lymphoma that might have reached these areas, chemotherapy such as methotrexate and cytarabine may be injected directly into the CSF. This is called intrathecal chemotherapy.
- Bendamustine is a newer chemotherapeutic agent can be used in combination with anti-CD20 mainly in low-grade or indolent B-cell lymphomas or lymphoproliferative disorders such as follicular lymphoma or mantle cell lymphoma. Older patients also tolerate this chemotherapy well.
- Side effects include:
- Loss of appetite
- Nausea
- Oral ulcer
- Hair loss
- Diarrhoea
- Weakened immune system
Steroid therapy
- Corticosteroids (Prednisolone is the most commonly used) are often given orally with chemotherapy as part of the lymphoma therapy. It may also alleviate symptoms such as nausea.
- Side effects:
- Indigestion, epigastric pain and peptic ulcer disease
- Increased appetite
- Restlessness/ Increased energy
- Difficulty in sleeping
- High blood sugar levels
- Risk of infections
- Reactivation of tuberculosis
- Reactivation of hepatitis B-virus (prophylaxis with antiviral is necessary in all hepatitis B carriers)
- Osteoporosis
Radiotherapy
- External beam radiotherapy (EBRT) releases targeted high-energy rays at the tumour to destroy cancer cells while causing minimum effects to normal ones.
- Before your EBRT treatment starts, your radiation team will take careful measurements to find the correct angles for aiming the radiation beams and the proper dose of radiation with the aid of CT, PET, or magnetic resonance imaging (MRI) scans. Casts, body molds, and head rests may be made to hold you in the same position for each treatment. Blocks or shields may be made to protect other parts of your body. You may be asked to hold your breath for a short time. The goal is to focus the radiation on the cancer to limit the effect on healthy tissues.
- Most often, EBRT treatments are given 5 days a week with a break at the weekend for several weeks. The procedure itself is painless. Each treatment lasts only a few minutes, although the setup time – getting you into place for treatment – usually takes longer.
- Side effects:
- Tiredness
- Skin changes over the targeted area (e.g. Redness, blistering and peeling)
- Other side effects may depend on the specific treated area
Radiotherapy alone is not the mainstay nowadays for treating lymphomas.
Chemotherapy and radiotherapy may be used sequentially in order to increase the remission rates in certain subtypes of lymphomas such as Stage I or II Classical Hodgkin lymphoma.
Radiotherapy may also be used to help control symptoms such as pain, treat bulky diseases as well as disease recurring in only group of lymph nodes.
Immunotherapy
Immunotherapy is the use of medicines to help a person’s immune system better recognise and destroy cancer cells. Immunotherapy can be used to treat some people with lymphoma.
Using these targeted anti-cancer drugs not only has better efficacy, but also reduces collateral damage to unaffected areas of the body.
Monoclonal antibodies
- Monoclonal antibodies attach to the specific biomarkers on lymphoma cells.
- Anti-CD20: Rituximab, Obinutuzumab, Ofatumumab
- Once in the body, the antibodies Rituximab Obinutuzumab , or Ofatumumab binds to CD20 on the surface of most B type cancer cells, causing cell death and ultimately destroying the tumour through a series of immune response.
- Good treatment response has been shown
- Anti-CD20 therapy in combination with multi-agent chemotherapy is an important measure for treating B-cell lymphomas.
- Anti-CD20 therapy and chemotherapy combination may be given with radiotherapy.
|
Drug Name
|
Indications(s)
|
|
Rituximab
|
- Used along with chemotherapy for some types of non-Hodgkin lymphoma
- May be used by itself
|
|
Obintuzumab
|
- Used along with chemotherapy for:
- Small lymphocytic lymphoma/ chronic lymphocytic lymphoma
- Follicular lymphoma
|
|
Ofatumumab
|
- Small lymphocytic lymphoma/ chronic lymphocytic lymphoma or follicular lymphoma
- No longer responding to other treatments
|
- Administration: given intravenously, often over several hours
- Common side effects: infusion reaction (itching, chills, fever, nausea, rashes, fatigues, and headaches. Serious reactions: chest pain, heart racings, swelling of the face and tongue, cough, trouble breathing, feeling dizzy or lightheaded, and feeling faint).
- Rituximab
- Administration: given intravenously, on the first day of each chemotherapy cycle.
- Another formulation can be given under the skin for 5-7 minutes.
- Brentuximab vedotin
- An antibody drug conjugate against CD30 attached to a cytotoxin/ chemotherapy drug called vedotin
- Usually used for relapsed CD30-positive classical Hodgkin lymphoma, anaplastic large cell lymphoma or other CD30-expressing lymphomas.
- Can also be used upfront in high-risk, stage III or IV, or recurring classical Hodgkin Lymphoma replacing Bleomycin in the regimen “ABVD”
- Can be used to treat some types of T-cell lymphoma, either as the first treatment (typically along with chemotherapy) or if the lymphoma has come back after other treatments.
- Administration: given intravenously, usually every 2 or 3 weeks
- Common side effects: nerve damage, low blood cell counts (increased risk of infection, fatigue, easy bruising and bleeding), fatigue, fever, nausea and vomiting, infections, diarrhoea
- Polatuzumab vedotin
- An antibody drug conjugate targeting CD79a attached to a chemotherapy drug called vedotin
- Can be used in patients with relapsed or refractory Diffuse Large B-cell lymphoma and is used in combination with Rituximab and Bendamustine.
- Recently proved to be effective when used upfront replacing vincristine in R-CHOP.
- Administration: given intravenously, typically every 3 weeks
- Common side effects: numbness or tingling of hands/feet (peripheral neuropathy), low blood counts (increased risk of infection, fatigue, easy bruising and bleeding), fatigue, fever, decreased appetite, diarrhoea, and pneumonia
- Anti-CD19: Tafasitamab, Loncastuximab tesirine
- CD19 is a protein on the surface of B lymphocytes.
- Tafasitamab
- An antibody that can be used along with lenalidomide to treat diffuse large B-cell lymphoma that has come back or is no longer responding to other treatments, in people who cannot have a stem cell transplant for some reason.
- Administration: given intravenously, typically about once a week for the first few months, and then once every two weeks
- Side effects: infusion reactions (chills, flushing, headache, or shortness of breath) during infusion, low blood cell counts (increased risk of bleeding and serious infections), feeling tired or weak, loss of appetite, diarrhoea, cough, fever, and swelling in the hands or legs.
- Loncastuximab tesirine
- An antibody drug conjugate targeting CD19 linked to a chemotherapy drug called tesirine
- Can be used by itself to treat some types of large B-cell lymphoma (including diffuse large B-cell lymphoma) after at least 2 other treatments (not including surgery or radiation) have been tried.
- Administration: given intravenously, once every 3 weeks
- Common side effects: abnormal liver function tests, low blood counts, feeling tired, rash, nausea, and muscle and joint pain
- More serious side effects: infection; fluid collection in the lungs, around the heart, or in the abdomen (belly); very low blood counts; and very severe skin reactions when out in the sun
- Anti-CD52: Alemtuzumab
- An antibody used in some cases of small lymphocytic lymphoma/ chronic lymphocytic lymphoma and some types of peripheral T-cell lymphomas.
- Administration: given intravenously, usually 3 times a week for up to 12 weeks
- Common side effects: fever, chills, nausea, rashes and very low white blood cell counts which increases the risk for serious infections
- Rare serious side effects: stroke, tears in blood vessels in the head and neck
- Bispecific T-cell engagers (BiTEs)
- Newer antibodies designed to attach to two different targets. Once in the body, one part of the antibody attaches to the CD3 protein on immune T cells. Another part attaches to a target on lymphoma cells, such as the CD20 protein. This brings the two cells together, which helps the immune system attack the lymphoma cells.
|
Drug Name
|
Indication(s)
|
Administration
|
|
Mosunetuzumab
|
Follicular lymphoma that has returned or that is no longer responding after treatment with at least 2 other types of drugs
|
Given intravenously, typically once a week for the first 3 weeks, then once every 3 weeks
|
|
Epcoritamab
|
- Diffuse large B-cell lymphoma or other high-grade B-cell lymphomas
- Follicular lymphoma
- Typically after other treatments have been tried
|
Given subcutaneously (injection under the skin), usually once a week for the first 3 months, then once or twice a month
|
|
Glofitamab
|
- Diffuse large B-cell lymphoma or large B-cell lymphoma arising from follicular lymphoma
- Typically after two or more other treatments have been tried
|
Given intravenously, typically once a week for the first 3 weeks, then once every 3 weeks
|
- Side effects: feeling tired, muscle or bone pain, rash, fever, nausea, diarrhoea, and headaches
- Serious side effects:
- Infusion reaction (itching, chills, fever, nausea, rashes, fatigues, and headaches)
- Serious reactions: chest pain, heart racings, swelling of the face and tongue, cough, trouble breathing, feeling dizzy or lightheaded, and feeling faint,
- Cytokine release syndrome (high fever and chills, muscle weakness, trouble breathing, low blood pressure, a very fast heartbeat, headache, nausea or vomiting, and feeling dizzy, lightheaded, or confused)
- Most often within the first day after treatment
- Can be serious or even life-threatening
- Nervous system problems (headaches, numbness or tingling in the heads or feet, feeling dizzy or confused, trouble speaking or understanding things, memory loss, abnormal sleep patterns, tremors, or seizures)
- Serious infections
- Low blood cell counts
- Tumour flare (tender or swollen lymph nodes, chest pain, cough, trouble breathing, or pain or swelling around a known tumour)
Immune checkpoint inhibitors
- A form of immunotherapy that enables the patients’ own immune cells called Tcell to recognise and kill the lymphoma cells by inhibiting programmed death-1 (PD-1).
- Examples include Nivolumab and Pembrolizumab.
- They are the most effective in patients with relapsed or refractory classical Hodgkin lymphoma.
- Nivolumab may also be an option given along with chemotherapy as part of the first treatment for advanced (stage III or IV) classic Hodgkin lymphoma.
- Pembrolizumab can be used to treat primary mediastinal large B-cell lymphoma that has not responded to or has come back after other treatments.
- Administration: given intravenously, typically every 2, 3, or 6 weeks
- Possible side effects: fatigue, fever, cough, nausea, itching, skin rash, loss of appetite, joint pain, constipation, diarrhoea
- Rare but serious side effects: infusion reactions (fever, chills, flushing on the face, rash, itchy skin, feeling dizzy, wheezing, and trouble breathing), autoimmune reactions (serious or even life-threatening problems in the lungs, intestines, liver, hormone-making glands, kidneys, or other organs)
Immunomodulating drugs: Thalidomide and Lenalidomide
- Thought to work against certain cancers by affecting parts of immune system, although exactly how they work is not clear.
- Used to help treat certain types of lymphoma, usually after other treatments have been tried.
- Can be given with or without rituximab, or along with tafasitamab
- Administration: taken orally, once every day
- Side effects: low white blood cell counts (increased risk of infection), neuropathy (painful nerve damage), increased risk of serious blood clots (that start in the leg and can travel to the lungs) especially with thalidomide
- Thalidomide side effects: drowsiness, fatigue, and severe constipation
- Can cause severe birth defects if taken during pregnancy
Chimeric Antigen Receptor (CAR) T-cell therapy (a form of cellular immunotherapy)
- First, the patient’s T-cells are “extracted” or “harvested”. The patient’s T-cells are then “genetically engineered” or “educated” to recognise the specific cell marker on the lymphoma cell (most commonly CD19 in diffuse large B-cell lymphoma). The “educated” T-cells (CAR-T cells) are multiplied in the lab and infused back to the patient to treat the lymphoma.
- Chemotherapy is given to prepare your body to accept the CAR T-cells before they are given to you.
- Indications:
|
Drug Name
|
Indication(s)
|
|
Axicabtagene ciloleucel
|
- Large B-cell lymphoma (including diffuse large B-cell lymphoma, primary mediastinal large B-cell lymphoma, high grade B-cell lymphoma, and diffuse large B-cell lymphoma arising from follicular lymphoma)
- Has not responded to initial treatment with chemotherapy plus immunotherapy, or that comes back within a year of this treatment
|
|
Tisagenlecleucel
|
- Diffuse large B-cell lymphoma, high grade B-cell lymphoma, and diffuse large B-cell lymphoma arising from follicular lymphoma, as well as follicular lymphoma
- Has not responded to or has come back after other therapies, after trying at least two other kinds of treatment
|
|
Lisocabtagene maraleucel
|
- Diffuse large B-cell lymphoma, primary mediastinal large B-cell lymphoma, high grade B-cell lymphoma, follicular lymphoma, mantle cell lymphoma, and small lymphocytic lymphoma/chronic lymphocytic leukaemia
- After other kinds of treatment have been tried
|
|
Brexucabtagene autoleucel
|
- Mantle cell lymphoma
- Has come back or is no longer responding to other treatments
|
- Side effects: cytokine release syndrome (fever, chills, headache, nausea and vomiting, trouble breathing, very low blood pressure, a very fast heart rate, swelling, diarrhoea, feeling very tired or weak, and other problems); neurological (nervous system problems such as confusion, trouble speaking, seizures, tremors, or changes in consciousness)
- Serious side effects: severe infections, low blood cell counts, weakened immune system
Targeted therapy
- Proteasome inhibitor: Bortezomib
- Works by stopping enzyme complexes (proteasomes) in cells from breaking down proteins that are important for keeping cell division under control.
- Helpful in treating some types of non-Hodgkin lymphoma
- Administration: given intravenously or under the skin, typically twice a week for 2 weeks, followed by a rest period
- Side effects: low blood cell counts (increased risk of infection, fatigue, easy bruising and bleeding), nausea, loss of appetite, nerve damage
- Histone deacetylase (HDAC) inhibitor: Belinostat
- Affects genes that are active inside cancer cells by affecting histone proteins, which interact with chromosomes
- Belinostat can be used to treat a specific type of non-Hodgkin lymphoma, peripheral T-cell lymphomas, usually after at least one other treatment has been tried.
- Administration: given intravenous, usually once every day for 5 days in a row, repeated every 3 weeks
- Common side effects: nausea, vomiting, tiredness, anaemia (fatigue)
- Bruton tyrosine kinase (BTK) inhibitors
- BTK is a protein that normally helps some lymphoma cells (B cells) grow and survive. BTK inhibitors can be helpful in treating some types of B-cell non-Hodgkin lymphomas.
- Administration: taken orally, typically once or twice a day
|
Drug Name
|
Indication(s)
|
|
Ibrutinib
|
- Chronic lymphocytic leukaemia/ small lymphocytic lymphoma
- Rare low-grade B-cell lymphomas that express the gene called “MYD88” (examples include Waldenstöm macroglobulinaemia and marginal zone B-cell lymphoma)
|
|
Acalabrutinib
|
- Mantle cell lymphoma
- Chronic lymphocytic leukaemia/ small lymphocytic lymphoma
|
|
Zanubrutinib
|
- Mantle cell lymphoma or marginal zone lymphoma, typically after at least one other treatment has been tried
- Chronic lymphocytic leukaemia/ small lymphocytic lymphoma
- Waldenström macroglobulinaemia
|
|
Pirtobrutinib
|
- Mantle cell lymphoma
- Chronic lymphocytic leukaemia/ small lymphocytic lymphoma
- Typically after at least 2 other treatments (including another BTK inhibitor) have been tried
|
- Common side effects: headache, diarrhoea, bruising, feeling tired, muscle and joint pain, cough, rash, and low blood cell counts
- Less common side effects: bleeding, infections, heart rhythm problems (such as atrial fibrillation), increased risk of skin or other cancers
- Bcl-2 inhibitor: Venetoclax
- Usually used in combination with an anti-CD20.
- Administration: taken orally, once every day
- Common side effects: low blood cell counts (increased risk of infection, fatigue, easy bruising and bleeding), diarrhoea, nausea, upper respiratory tract infection, cough, muscle and joint pain, oedema
- Phosphatidylinositol 3-kinase (PI3K) inhibitor: Duvelisib
- Phosphatidylinositol 3-kinases (PI3Ks) are a family of proteins that send signals in cells that can affect cell growth. PI3K inhibitors can be helpful in treating some types of non-Hodgkin lymphoma.
- Duvelisib can be used to treat small lymphocytic lymphoma, typically after other treatments have been tried.
- Administration: taken orally, twice a day
- Common side effects: diarrhoea, fever, fatigue, nausea, cough, pneumonia, belly pain, joint/muscle pain, rash, low red blood cell counts (anaemia), low levels of certain white blood cells (neutropenia)
- Less common but serious side effects: liver damage, severe diarrhoea, lung inflammation (pneumonitis), serious allergic reactions, and severe skin problems
- EZH2 inhibitor: Tazemetostat
- EZH2 is a protein known as a methyltransferase that normally helps some cancer cells to grow.
- Tazemetostat can be used to treat follicular lymphomas with an EZH2 gene mutation, after other treatments have been tried.
- Tazemetostat can also be used to treat follicular lymphomas without an EZH2 gene mutation, if there are no other good treatment options available.
- Administration: taken orally, typically twice a day
- Common side effects: bone and muscle pain, feeling tired, nausea, belly pain, and cold-like symptoms
- Increased risk of developing some types of blood cancers
- Nuclear export inhibitor: Selinexor
- The nucleus of a cell holds most of what the cell needs to make the proteins so it can function and stay alive. A protein called XPO1 helps carry other proteins from the nucleus to other parts of the cell to keep it working.
- Selinexor works by blocking the XPO1 protein hence the lymphoma cell cannot move proteins outside of its nucleus and dies.
- Selinexor is used in patients with diffuse large B-cell lymphoma whose cancer has come back, or who have been treated with and no longer respond to at least 2 other diffuse large B-cell lymphoma drugs.
- Administration: taken orally, on the first and third day of each week
- Common side effects: feeling tired, nausea, diarrhoea, loss of appetite, weight loss, vomiting, constipation, and fever
- More serious side effects: low platelet counts (easy bruising and bleeding), low white blood cell counts (increased risk of infection), low blood sodium levels (cramps and twitching), infection, dizziness, and more severe gastrointestinal problems
Choosing the right therapy
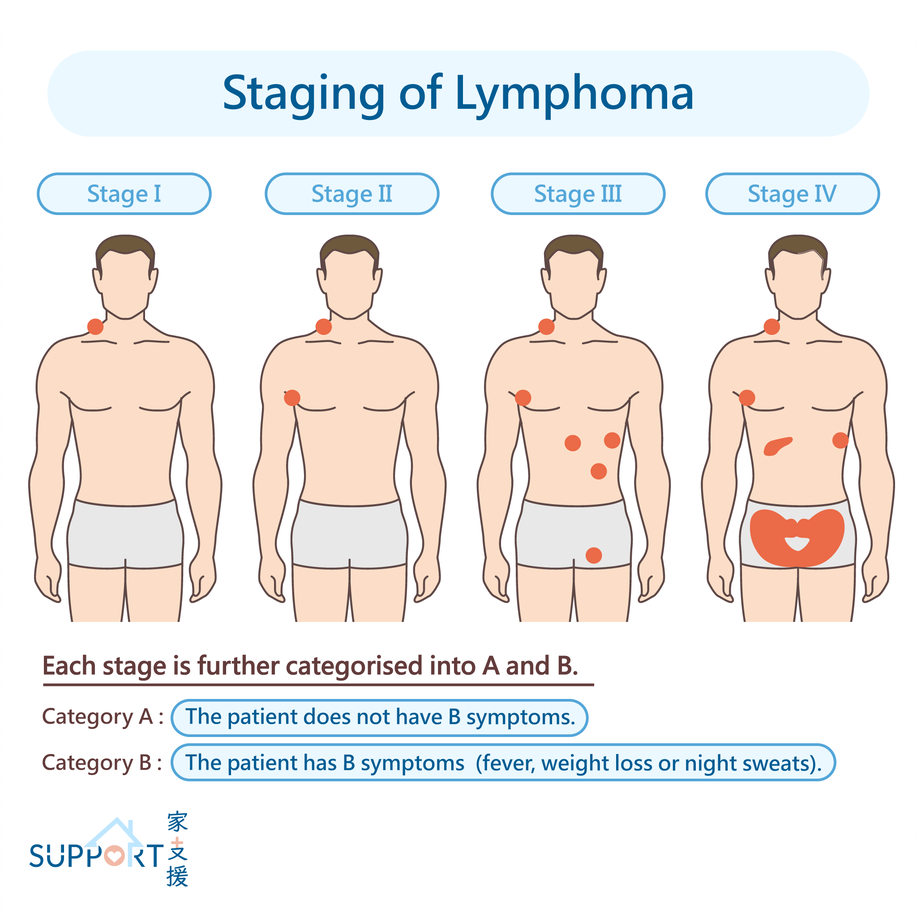
- An appropriate treatment plan must be devised according to the subtype, stage and the status of lymphoma as well as the patient’s condition and preference.
Hodgkin Lymphoma
- Early stage (I, II): Combination of chemotherapy (e.g. Adriamycin-BleomycinVinblastine-Dacarbazine = ABVD) with or without radiotherapy. Please note that Brentuximab vedotin may be used in place of Bleomycin
- 2-4 cycles of chemotherapy
- May be followed by involve-field radiotherapy usually in patients with bulky disease.
- More intense chemotherapy e.g. ABVD for 4-6 cycles may be given for less favourable disease e.g. bulky disease, three or more different areas of lymph nodes involved, extranodal involvement, presence of B symptoms
- If a person cannot have chemotherapy because of other health issues, radiation therapy alone may be an option.
- The monoclonal antibody rituximab may be given along with the chemotherapy.
- 80-90% of patients can be cured
- Significantly reduces the risk and complications of treatment
- For patients with early-stage nodular lymphocyte predominant Hodgkin lymphoma without any B symptoms, involved site radiation therapy is often the only treatment needed. Another option for some patients may be to have the lymphoma watched closely at first, and then start treatment when symptoms appear.
- Advanced stage (III, IV): Multi-agent-chemotherapy (e.g. ABVD or Escalated BEACOPP) with or without radiotherapy and/or rituximab
- The current chemotherapy regimen is very effective.
- Some patients without B symptoms may be given rituximab alone.
- 60-70% of patients can be cured.
Non-Hodgkin Lymphoma
- Treatment methods are more complex, and they vary depending on the exact classification of lymphoma.
- Indolent or low-grade B-cell lymphomas:
- Often in an advanced stage when it is diagnosed, disease progression is slow. With treatment advances, most subtypes can be cured or achieve long-term remission.
- Anti-CD20 in combination with chemotherapy [CyclophosphamideDoxorubicin (Hydroxydaunorubicin)-Vincristine -Prednisolone=CHOP] (R-CHOP) in 3-weekly cycles is the mainstay of treatment.
- Asymptomatic patients may only have anti-CD20.
- Sometimes radiotherapy is used to shrink the lymphoma in an area and reduce symptoms.
- Rarely, surgery may be performed to remove the affected organs, for example in Burkitt lymphoma, splenic marginal zone B-cell lymphoma, non-gastric MALT lymphoma.
- Aggressive or high-grade B-lymphomas:
- Rapid disease progression, start treatment as soon as possible
- 6-8 cycles of chemotherapy
- In the case of diffuse large B-cell lymphoma, the patient can receive a combination of Rituximab and chemotherapy [CyclophosphamideDoxorubicin (Hydroxydaunorubicin)-Vincristine-Prednisolone=CHOP] (RCHOP). The antibody drug conjugate polatuzumab vedotin may be added to the R-CHOP combination. Other regimens that include chemotherapy and rituximab may be options as well.
- Patients who have a higher risk of having the lymphoma coming back at a later time in the tissues around the brain and spinal cord may also be treated with chemotherapy injected into the spinal fluid (called intrathecal chemotherapy). Another option is to give high doses of methotrexate intravenously since it can pass into the spinal fluid.
- In the case of follicular lymphoma, besides R-CHOP, another option may be the immunotherapy drug lenalidomide, plus a monoclonal antibody.
- In the case of chronic lymphocytic leukaemia/ small lymphocytic lymphoma, the most common options for first-line treatment include a targeted drug – either a BTK inhibitor, such as ibrutinib, acalabrutinib, or zanubrutinib, or the BCL-2 inhibitor venetoclax, along with a monoclonal antibody such as obinutuzumab or rituximab, or with a second targeted drug.
- In the case of mantle cell lymphoma, other chemotherapy regimens may be used, such as LyMA, NORDIC, TRIANGLE, Hyper-CVAD. Sometimes another type of drug, such as a targeted drug like acalabrutinib or bortezomib, or the immunotherapy drug lenalidomide may be included in the treatment. If the lymphoma responds well to the initial treatment, a haematopoietic stem cell transplant (HSCT) may be a good option. This is often followed by a targeted drug (a BTK inhibitor) plus rituximab for several years.
- Sometimes, radiotherapy is given after chemotherapy usually if the lymphoma was only in one area of the body. It may also be used if the lymph nodes were very bulky before you had chemotherapy. Radiation may be used to reduce symptoms if some lymph nodes are very large from the lymphoma, most often for patients who are too sick to be treated with chemotherapy.
- Early stage: Curative rate is 70-80%
- Advanced stage: Curative rate is 30-50%
- T-cell or NK/T-cell lymphomas
- Treatment is more complicated and usually involve multi-agent chemotherapy, such as CHOP, CHOEP, EPOCH, CHP plus the antibodydrug conjugate brentuximab vedotin if the lymphoma cells have the CD30 protein, HyerperCVAD alternating with high-dose methotrexate and cytarabine.
- Because of the risk of spread to the brain and spinal cord, a chemotherapy drug such as methotrexate may also be given into the spinal fluid.
- For people who can’t tolerate intense chemotherapy, a single chemotherapy or immunotherapy drug might be an option.
- If the lymphoma is only in one area, radiation therapy may be an option.
- Rarely, surgery may be performed to remove the affected organs, for example in enteropathy-associated T-cell lymphoma, anaplastic large cell lymphoma.
- Some doctors suggest maintenance chemotherapy for up to 2 years after the initial treatment to reduce the risk of recurrence. High-dose chemotherapy followed by a haematopoietic stem cell transplant (HSCT) may be another option if the lymphoma responds to treatment.
- These lymphomas should be treated in hospitals and centres with expertise in these conditions.
- Anti-infectives may be given if the lymphoma is associated with an infectious source.
Relapsed or refractory lymphoma
- Low-grade non-Hodgkin lymphoma cannot usually be cured. It nearly always comes back or starts to grow again at some point after treatment. You can have further treatment to control the lymphoma. This can often keep patients feeling not well for long periods of time. For some patients with low-grade lymphoma, the doctor may suggest watch and wait i.e. monitoring the lymphoma with regular tests rather than starting more treatment straight away, especially if the lymphoma is not causing problems other than mildly swollen lymph nodes. Some people may never need treatment at all. For those who do, it may be years before treatment is needed.
- If lymphoma comes back, you may have one, or a combination of the following treatments:
- Chemotherapy – with different drugs that are usually stronger than the ones you had before. The regimen may or may not include rituximab.
- Targeted therapy and immunotherapy – you may have a different drug than you have had before
- Radiotherapy – may be used if lymphoma comes back in one group of lymph nodes of to relieve symptoms
- Haematopoietic stem cell transplant (HSCT)
- CAR-T therapy
- Hematopoietic stem cell transplantation (HSCT)
- High-dose or “myeloablative” chemotherapy sometimes with radiotherapy is used to “wipe off” any residual lymphomas. HSCT is not likely to be effective unless the lymphoma responds to chemotherapy.
- Stem cells from patient himself or herself (autologous transplant) or from another person, such as a sibling, unrelated donor, or umbilical cord blood (allogeneic transplant) are infused to the patients. The donors tissue type needs to match the patient’s tissue type as closely as possible to help prevent major problems with the transplant.
- In Autologous HSCT, the patient’s own stem cells are collected or “harvested” several times in the weeks beforehand. The cells are frozen and stored while the patient gets treatment (high-dose chemotherapy with or without radiation) and then are given back into the patient’s blood by an intravenous infusion.
- Autologous HSCT is the most commonly indicated in relapsed lymphomas that are chemosensitive achieving a second remission.
- Allogeneic HSCT is only done in very selected cases and is not the standard in lymphomas. Usually, in treating Hodgkin lymphoma, an allogenic transplant is used only if an autologous transplant has already been tried without success.
- The risk involved is relatively high
- Chimeric Antigen Receptor (CAR) T-cell therapy
- Indicated in patients with relapsed or refractory CD19-expressing diffuse large-B cell lymphoma or primary mediastinal large B-cell lymphoma that is still growing after 2 or more courses of treatment.
- This type of therapy can also be used in some forms of low-grade B-cell lymphomas such as follicular lymphoma that are refractory to multiple lines of chemotherapy.
- The procedure is relatively safe when done in specialised centres.
- Immune checkpoint inhibitors
- Nivolumab and pembrolizumab are very effective in patients with classical Hodgkin lymphoma that relapse after autologous HSCT.
How to look after yourself during treatment
Before starting any treatment, the doctor will explain the procedures, risks and side effects to the patient. Also, if you are young and want to plan a family, discuss issues on fertility and conception before starting treatment. Your doctor will refer you to a fertility specialist for further counselling and methods to preserve fertility as applicable to your condition.
During treatment, you should:
- Follow your doctor’s instructions, the medicine as prescribed and have regular follow ups
- Keep a balanced diet
- Balance rest periods with moderate exercise
- Maintain good personal hygiene
- Rooms, clothes and utensils should be cleaned frequently
- Eat only thoroughly cooked food
- Stay away from crowded places