Surgical treatment
Oesophagectomy
Oesophagectomy refers to the resection of the oesophagus, which is mainly performed for malignancy of the oesophagus. Occasionally, it is also indicated in benign conditions, like perforation and non-malignant narrowing (e.g. corrosive stricture). Following oesophagectomy, the stomach will be pulled up in order to regain the continuity of the gastro-intestinal tract. In certain cases, a segment of the large bowel is required to work as the conduit for reconstruction.
The operation is carried out under general anaesthesia with selective ventilation of the lungs. Epidural anaesthesia or patient-control-anaesthesia is frequently applied to reduce post-operative pain in view of the thoracotomy wound.
Conventionally, oesophagectomy includes three phases:
- Surgical resection of the oesophagus
- Mobilisation of the stomach and keeping the blood supply with it
- Anastomosis to maintain continuity of the gastro-intestinal tract
Open surgical approach results in incisions over abdomen, the chest and neck. Nowadays, laparoscopic and thoracoscopic dissection can be performed as minimal invasive procedures. The surgery takes at least 5-6 hours to complete. After surgery, ICU care for ventilatory support and monitoring is the routine practice. Early ambulation and early oral feeding are advisable depending on the progress of recovery. Post-operative intensive care is absolutely indicated. Specific complications related to oesophagectomy include:
- Intra-operative bleeding in view of the extensive field of dissection and the nearby major vessels.
- Anastomotic leakage because of tension to anastomosis and / or impaired blood supply.
- Chylothorax as a result of damage to lymphatic system.
- Chest infection or pneumonia. The majority of patients developing this complication are heavy smokers with poor respiratory function. The thoracotomy wound and single lung ventilation further hinder recovery. Indeed, sputum retention and chest complications are still the most likely causes of surgical failure.
Neoadjuvant/adjuvant treatment
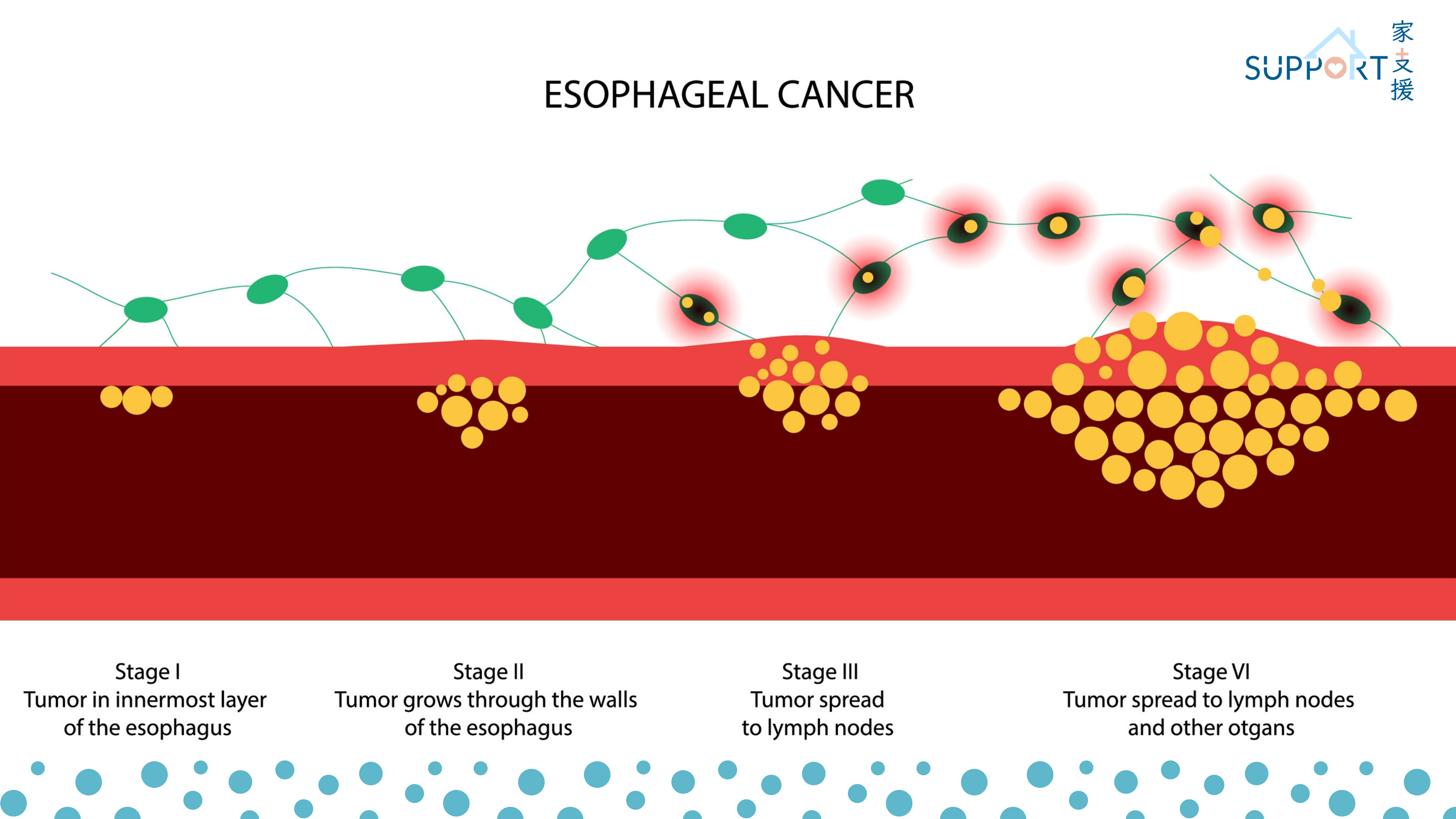
Neoadjuvant treatment is an anti-cancer treatment given before definitive local treatment, such as surgery. For oesophageal tumours that are large or with nodal metastases, neoadjuvant treatment may be considered before the surgery to shrink the tumour (downstaging), thereby, increasing the possibility of a clean surgery (negative resection margins). Additional treatment may be considered after surgery (adjuvant treatment) for certain cases.
Neoadjuvant chemoradiation
Chemoradiation is commonly used for stage II to III oesophageal squamous cell carcinomas before surgery. The treatment is given 5 days a week and lasts over a
course of 5 weeks. Chemotherapy will be given during external beam radiation therapy (EBRT) with weekly injection for 5 cycles, commonly used drugs include
paclitaxel and carboplatin. The treatment can be delivered in an outpatient clinic without the need of hospital admission.

Figure: Radiotherapy planning for oesophageal cancer using CT scan
After completing the treatment, the disease will be re-evaluated by endoscopy and imaging to assess the response of the tumour. Surgery will be arranged within 1-2 months after completion of chemoradiation.
The resected tumour will be sent for examination under microscopy. If residual tumour cells are not found in the resected tumour (complete remission after chemoradiation), there will be no additional treatment required after surgery. For patients with residual disease noted in the resected cancer, recent clinical trial has shown that the use of immunotherapy after surgery (adjuvant nivolumab) will increase chances of survival.
For some patients with residual disease left behind in surgery, usually due to the tumour being adjoint to important structures like the trachea or bronchus, additional radiation may be considered. Follow up treatment after surgery should be individualised depending on surgical and pathological findings, as well as the progress of recovery and health condition of the patient.
Neoadjuvant Chemotherapy
Squamous cell carcinomas of oesophagus
For squamous cell carcinoma that are long or with extensive nodal metastases, such as having spread to the neck or abdominal nodes, it may not be feasible to cover all sites noted on imaging in the radiotherapy field. For such patients, chemotherapy may be performed alone without radiation. The chemotherapy used will be more intensive, with combination of 2-3 drugs. Examples of combination chemotherapy include PF [Cisplatin-5-fluorouracil (5FU)] and TPF (cisplatin, 5-FU and docetaxel). After 2-3 cycles of chemotherapy, re-evaluation will be performed to assess its operability.
Adenocarcinomas of gastroesophageal junction
Adenocarcinomas of gastroesophageal junction behaves more like stomach cancers and are managed similarly. These cancers are usually treated with peri-operative chemotherapy both before and after surgery.
Chemotherapy will consist of 3 drugs, 5-FU, oxaliplatin and docetaxel (FLOT), used every 2 weeks for 4 cycles, followed by re-evaluation. After surgery, another 4 cycles of the same chemotherapy will be given.
Definitive chemoradiation
Chemoradiation may be used as a definitive treatment without surgery for squamous cell carcinoma, especially for patients who are medically unfit or unable to afford surgery.
For oesophageal cancers in the neck that are close to the larynx, definitive chemoradiation may be considered as alternative to surgery in order to preserve the larynx.
Definitive chemoradiation will involve high dose radiation given daily for 5-6 weeks. Chemotherapy is commonly given during the course of radiation (2 cycles of cisplatin and 5-FU) and after completion of radiotherapy (another 2 cycles of cisplatin and 5- FU).