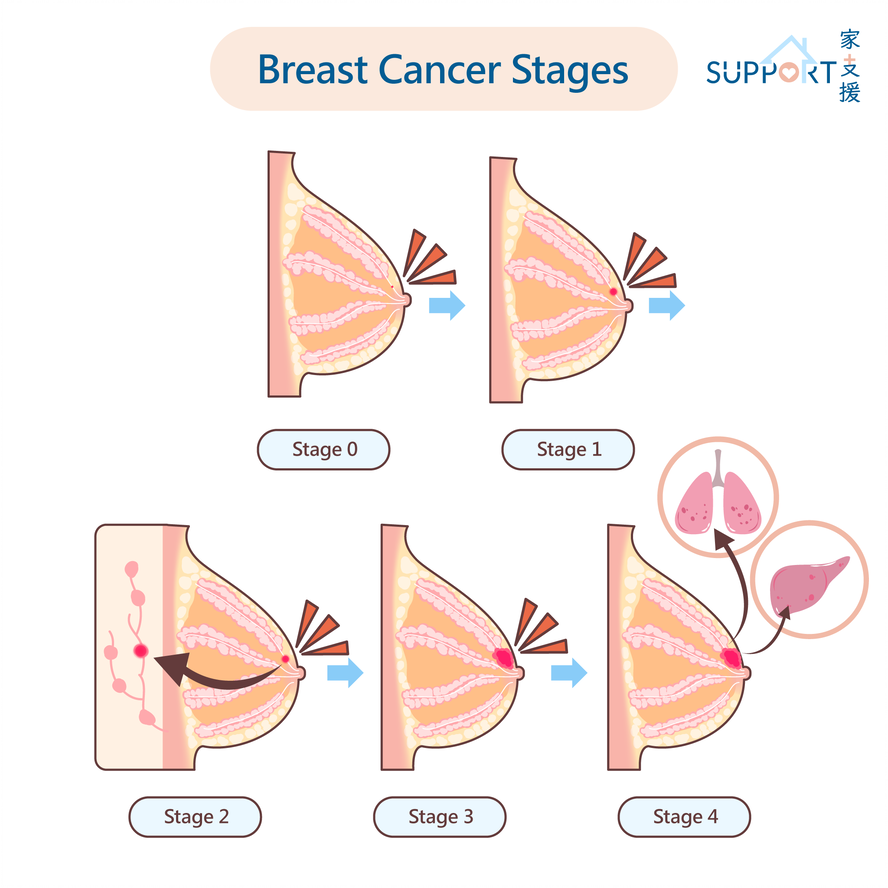
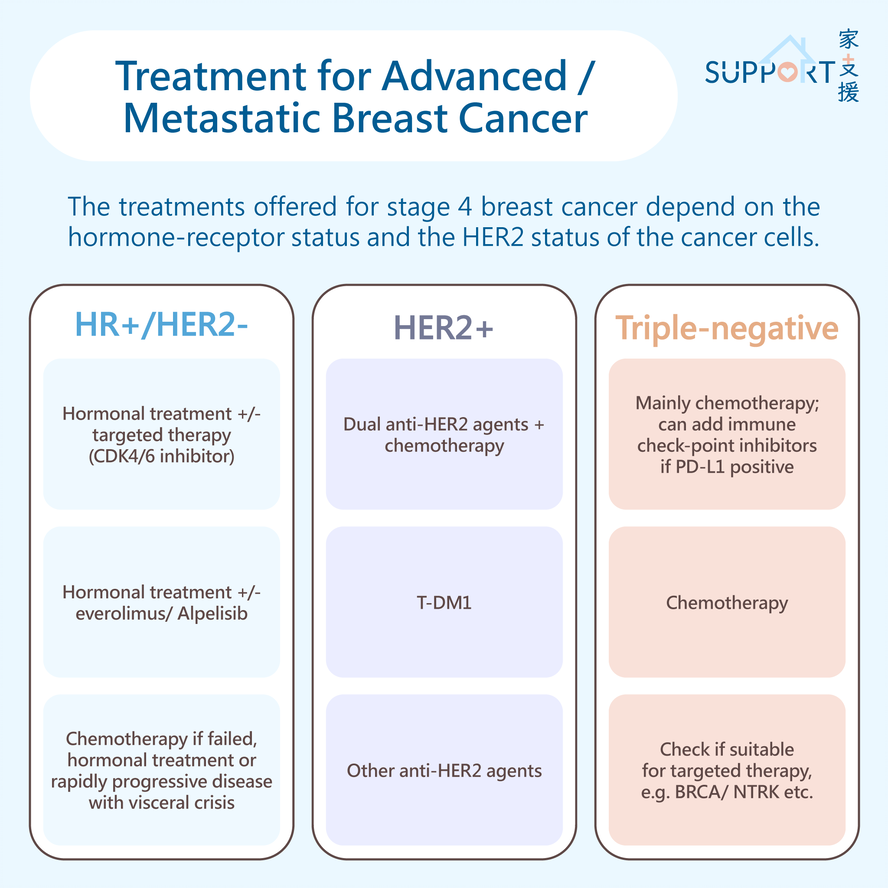
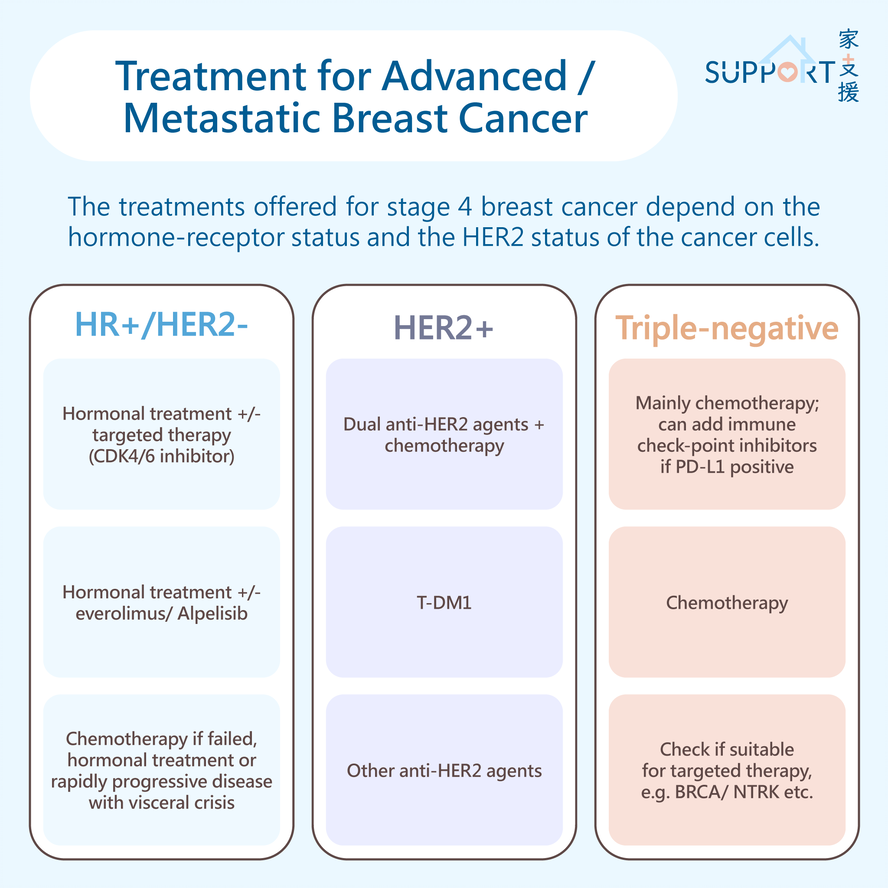
Advanced breast cancer, or metastatic breast cancer means that the breast cancer is not operable and has spread to other parts of the body. Treatments cannot completely cure metastatic breast cancer, but they can control it, sometimes for many years.
The treatments offered for stage IV breast cancer depend on the hormone-receptor status and the HER2 status of the cancer cells. They will also depend on where the cancer has spread to, whether it is causing any symptoms, and your overall health.
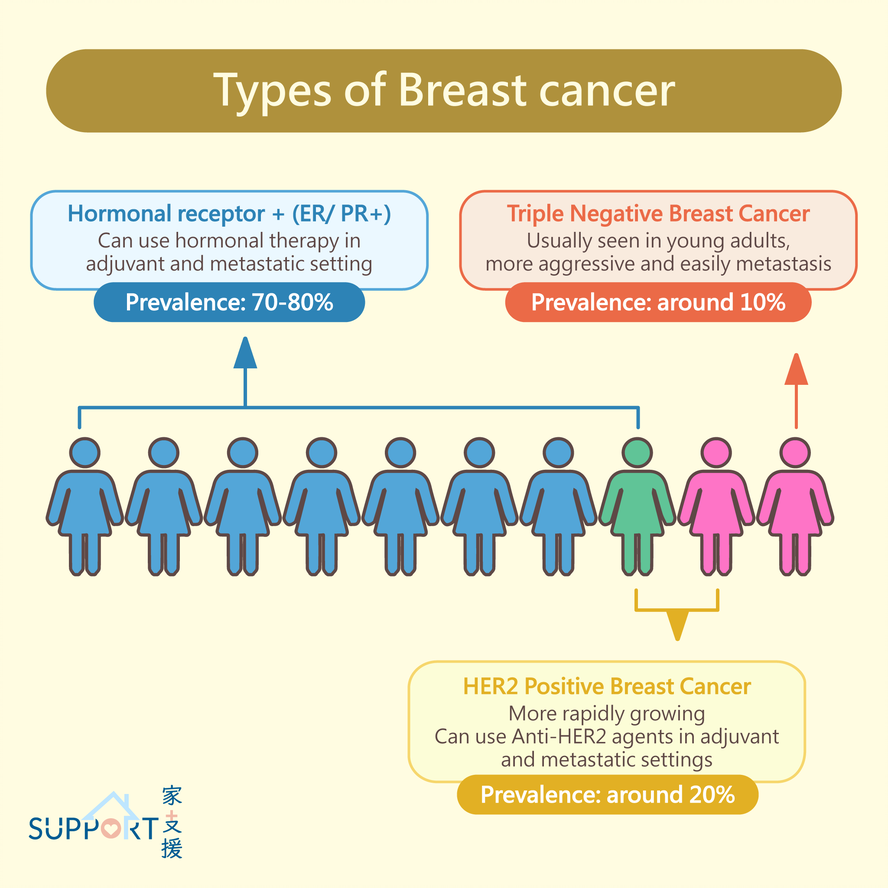
Hormonal receptor-positive, HER2-negative breast cancer (HR+/HER2-)
A. Hormonal therapy
- Hormonal therapy, also called endocrine therapy, is an effective treatment for breast cancer with ER+ or PR+.
- Options for hormonal therapy include:
- Tamoxifen
- Administration: taken daily orally
- Mechanism: Tamoxifen is a drug that blocks oestrogen from binding to breast cancer cells. This will inhibit the growth of cancer cells.
- Common side effects: hot flushes, vaginal discharge or bleeding; Very rare risks include a cancer of the lining of the uterus, cataracts, and blood clots.
- This treatment is an option for both premenopausal and postmenopausal women and for men.
- Aromatase inhibitors (AI): anastrozole, exemestane, and letrozole
- Administration: taken orally daily
- Mechanism: AIs decrease the amount of oestrogen produced by tissues other than the ovaries by blocking the aromatase enzyme. This enzyme changes androgen hormones into oestrogen when the ovaries stop producing oestrogen after menopause.
- Side effects: joint stiffness, sometimes with joint aches, hot flushes, vaginal dryness, an increased risk of osteoporosis and broken bones, and increased cholesterol levels.
- Used for post-menopausal women. Both premenopausal women and men can take AIs as long as they have ovarian suppression (see below). Women who have not gone through menopause should not take AIs without the injectable medication to block ovarian function, as they do not block the effects of estrogen made by the ovaries.
- Ovarian suppression
- Gonadotropin or luteinizing releasing hormone (GnRH or LHRH) agonists, examples include goserelin or leuprorelin
- Administration: subcutaneously in monthly (goserelin) or 3- monthly (leuprorelin) dose
- Mechanism: Stop the ovaries from producing oestrogen, causing temporary menopause
- Ovarian suppression is commonly used as a part of treatment for HR+ metastatic breast cancer in women who have not been through menopause. It is used with tamoxifen, an AI or fulvestrant.
- Other methods of ovarian suppression: surgery to remove both ovaries, radiotherapy to the pelvis to stop the ovarian function.
- Fulvestrant
- Administration: monthly injection into muscles (2 injections are given every 2 weeks for the first 3 doses and then continued monthly)
- Mechanism: Fulvestrant is a selective oestrogen receptor downregulator (SERD) that blocks the ability of oestrogen to attach to oestrogen receptors (ER).
- Fulvestrant is only for women who have been through menopause or who are also receiving a shot to stop their ovarian function
- Elacestrant
- Administration: taken daily orally
- Mechanism: Elacestrant is an oral selective estrogen receptor degrader (SERD). It works by both blocking and breaking down the estrogen receptor, thereby inhibiting the growth of HR+/HER2- breast cancer cells.
- Elacestrant is for patients with ESR1 mutations and had progression after at least one line of hormonal therapy.
- Side effects: Hot flashes and/or night sweats, headache, nausea, malaise, loss of appetite, joint pain, raised blood cholesterol level
B. Targeted therapy for HR+/HER2- advanced breast cancer
- CDK4/6 inhibitors: Palbociclib/ Ribociclib/ Abemaciclib
- What are CDK4/6 inhibitors?
- CDK4/6 inhibitors interrupt the process through which breast cancer cells divide and multiply. To do this, they target specific proteins known as the cyclin-dependent kinases 4 and 6, abbreviated as CDK4/6.
- The CDK4/6 proteins, found both in healthy cells and cancer cells, control how quickly cells grow and divide. In metastatic breast cancer, these proteins can become overactive and cause the cells to grow and divide uncontrollably. CDK4/6 inhibitors interrupt these proteins in order to slow or even stop the cancer cells from growing.
- CDK4/6 inhibitors are used to treat metastatic breast cancers that are HR+/ HER2-.
- Examples of CDK4/6 inhibitors
- Palbociclib and Ribociclib
- Oral medication: taken once a day, 3 weeks on and 1 week off
- Abemaciclib
- Oral medication: taken twice a day, continuous dosing
- Side effects of CDK4/6 inhibitors
- nausea
- diarrhea
- fatigue
- low white blood cell counts (also called neutropenia)
- anaemia (low red blood cell counts)
- low platelet counts
- Specific side effects:
- Abemaciclib: Diarrhea (It can be severe in about 10 percent of patients)
- Ribociclib: Ribociclib can cause a heart problem known as QT interval prolongation. (The QT interval is a measurement made on an electrocardiogram, or EKG, which is used to record the electrical activity of the heart.) This can lead to a fast or irregular heartbeat, which may be life-threatening but it is very rare. Patients taking ribociclib need to have an EKG before initiating and 2 weeks after initiating treatment.
Other targeted agents for HR+/HER2- advanced breast cancer
- Everolimus
- Administration: taken orally, once a day
- Mechanism: Everolimus blocks the mammalian target of rapamycin (mTOR), the protein in cells that normally helps them grow the divide. Everolimus may also stop tumours from developing new blood vessels, which can help limit their growth.
- Everolimus is used with the AI exemestane for ER-positive, HER2-negative metastatic breast cancer that has grown despite treatment with another AI.
- Side effects: mouth sores, rash, diarrhea, and, rarely, an inflammation of the lungs called interstitial pneumonitis.
- Alpelisib
- Administration: taken orally, once a day
- Alpelisib is an option along with the hormonal therapy fulvestrant for some people with HR+, HER2-negative metastatic breast cancer that has a PIK3CA gene mutation that has grown during or after treatment with hormonal therapy.
- Side effects: diarrhea, rash, fatigue, decreased in blood cell count, nausea and vomiting, mouth sores, increased serum sugar level, deranged liver function
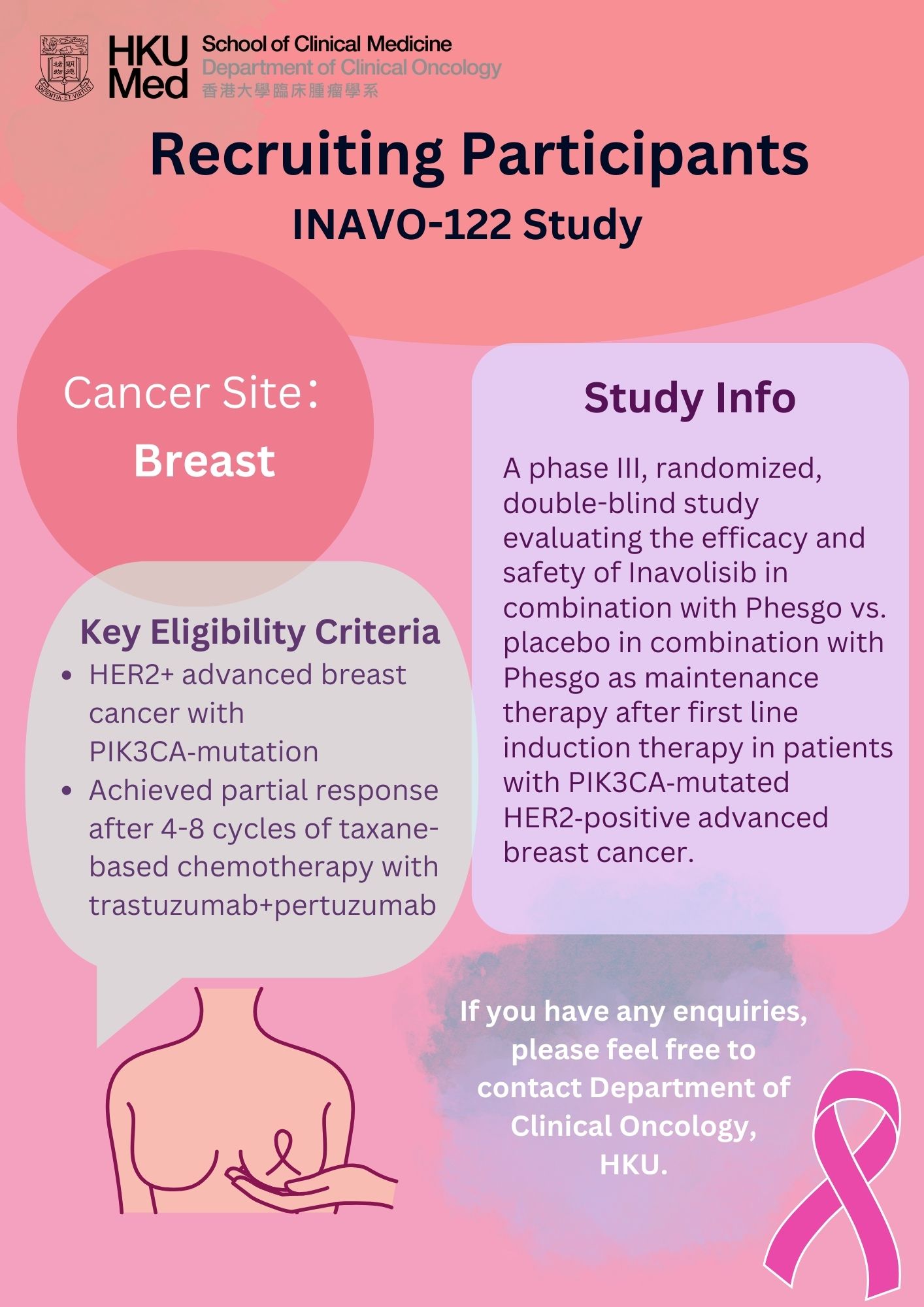
- Inavolisib
- Administration: taken orally, once a day
- Inavolisib has two main actions. First, it blocks a protein called PI3Kα that helps cancer cells grow. Second, it helps break down the mutated PI3Kα protein in cancer cells.
- Inavolisib is used in combination with palbociclib and fulvestrant. It is indicated for the treatment of adults with endocrine-resistant, PIK3CAmutated, HR+HER2-, locally advanced or metastatic breast cancer.
- Side effects: High blood sugar, sore mouth, diarrhea, malaise, electrolyte disturbance, low white cell counts.
- Capivasertib
- Administration: taken orally, twice a day for 4 days then rest for 3 days
- Capivasertib is a powerful inhibitor that blocks the AKT protein, which plays a crucial role in cancer cell growth and survival. It has shown significant anti-cancer effects in early research. The PI3K/AKT/mTOR pathway, which Capivasertib targets, is vital for cell survival, growth, and proliferation. This pathway interacts with estrogen receptor signaling, making it an important target for treating hormone-sensitive cancers.
- Capivasertib is used with fulvestrant for adult patients with HR+/HER2- locally advanced or metastatic breast cancer with one or more PIK3CA/AKT1/PTEN-alterations following progression on at least one endocrine-based regimen in the metastatic setting or recurrence on or within 12 months of completing adjuvant therapy.
- Side effects: high blood glucose level, diarrhea, skin rash or skin reactions, nausea, vomiting, mouth sores, loss of appetite, etc.
Antibody-drug Conjugates:
- Trastuzumab deruxtecan or T-DXD
- Administration: intravenously, given every 3 weeks
- This HER2-targeted treatment is a combination of a drug that is similar to trastuzumab, linked to a small amount of a strong chemotherapy. The trastuzumab biosimilar carries the chemotherapy to the HER2- positive cancer cells so it can kill the cancer cells and limit damage to healthy cells.
- T-DXD can be considered for patients with unresectable or metastatic hormone receptor–positive, HER2-low and HER2-ultralow breast cancer who previously received 1 or more endocrine therapies in the metastatic setting.
- Side effects: Nausea/ vomiting, tiredness, hair loss, loss of appetite, liver function impairment, low risk of interstitial lung disease (ILD), which causes scarring of the lungs, making it difficult to breathe or causing coughing.
- Sacituzumab govitecan
- Administration: Intravenously, given on day 1 and 8 every 21 days per cycle
- Sacituzumab govitecan is an ADC, which is a complex molecule composed of an antibody linked to a biologically active cytotoxic (anticancer) payload or drug. It is an option for patients with unresectable locally advanced or metastatic HR+, HER2-negative breast cancer who have received endocrine-based therapy and at least two additional systemic therapies in the metastatic setting.
- Common side effects: neutropenia, diarrhea, nausea and vomiting, and allergic reaction.
HER2-positive breast cancer (HER2+)
- In general, for a person with HER2+ metastatic breast cancer, there is almost always a HER2-targeted therapy being used along with another systemic therapy.
- Anti-HER2 targeted therapy includes:
- Trastuzumab
- Trastuzumab can be given in combination with chemotherapy (e.g. taxanes based) or hormonal therapy.
- Administration: every 3 weeks with intravenous infusion or subcutaneous injection
- Side effects: risk of heart problems in 2% to 5% of patients. Requires cardiac monitoring with echocardiogram or MUGA every 3 months.
- Pertuzumab
- Pertuzumab is given in combination with trastuzumab and chemotherapy (docetaxel, paclitaxel) as first-line therapy for HER2+ metastatic breast cancer as this combination can improve the survival of the patients.
- Administration: intravenous medication, given every 3 weeks
- Phesgo (combination of pertuzumab and trastuzumab in a single dose), a novel preparation, can be given by subcutaneous injection.
- Side effects: occasionally causes diarrhea and rash.
- Ado-trastuzumab emtansine or T-DM1
- T-DM1 is a combination of trastuzumab linked to very small amount of a strong chemotherapy. This allows the drug to deliver chemotherapy into the cancer cell while lessening the chemotherapy received by healthy cells, which usually means that it causes fewer side effects than standard chemotherapy.
- Administration: given intravenously every 3 weeks
- This is approved for the treatment of metastatic breast cancer for patients who have previously received trastuzumab and chemotherapy with either paclitaxel or docetaxel.
- Side effects: small risk of heart problems and liver abnormalities
- Trastuzumab deruxtecan or T-DXD
- Administration: intravenously, given every 3 weeks
- This HER2-targeted treatment is a combination of a drug that is similar to trastuzumab, linked to a small amount of a strong chemotherapy. The trastuzumab biosimilar carries the chemotherapy to the HER2-positive cancer cells so it can kill the cancer cells and limit damage to healthy cells.
- It is used for patients with unresectable or metastatic HER2- positive breast cancer who have received prior anti-HER2-based regimens.
- Side effects: Nausea/ vomiting, tiredness, hair loss, loss of appetite, liver function impairment, low risk of interstitial lung disease (ILD), which causes scarring of the lungs, making it difficult to breathe or causing coughing.
- Lapatinib
- Administration: oral medication, taken once a day
- Lapatinib and capecitabine (Xeloda) may be given to treat metastatic HER2-positive breast cancer when other types of chemotherapy or HER2-targeted therapies no longer work.
- Lapatinib and capecitabine (Xeloda) may be given to treat metastatic HER2-positive breast cancer when other types of chemotherapy or HER2-targeted therapies no longer work.
- Side effects: diarrhea, liver function impairment
- Neratinib
- Administration: oral medication, taken once a day
- Neratinib, in combination with capecitabine chemotherapy, can be considered for the treatment of advanced or metastatic HER2- positive breast cancer in patients who have already received 3 or more HER2-targeted therapies.
- Side effects: diarrhea, liver function impairment
- Tucatinib
- Administration: oral medication, taken twice a day
- Tucatinib, in combination with trastuzumab and capecitabine, is an option for patients with advanced unresectable or metastatic HER2-positive breast cancer, including patients with brain metastases, who have received one or more prior anti-HER2-based regimens in the metastatic setting.
- Side effects: Diarrhea, rashes, pain, swelling or blisters on the palms, mouth sores, decreased appetite, nausea and vomiting, tiredness, liver function impairment
Triple-negative breast cancer (HR-/HER2-)
Chemotherapy
- Chemotherapy is the major treatment modality for triple-negative breast cancer. With recent advances in novel medications, immunotherapy can be used together with chemotherapy in some patients with metastatic triple-negative breast cancer.
- Though having many new medications developed in recent years, chemotherapy still plays an important role in the treatment of metastatic breast cancer (all types).
- Chemotherapy for metastatic breast cancer can be given on many different schedules. It may be given once a week, once every 2 weeks (also called dose-dense), once every 3 weeks, or once every 4 weeks. Weekly schedules often include weeks off as a break.
- In general, chemotherapy is often given continuously as long as it is working against the cancer and the patient isn’t experiencing too many side effects.
- The best chemotherapy option for each patient depends on several factors, including the previous treatment received, potential side effects, the patient’s overall health, and the patient’s preferences.
- The following single drugs may be used:
- Doxorubicin/ epirubicin
- Paclitaxel/ docetaxel/ nab-paclitaxel
- Pegylated liposomal doxorubicin
- Capecitabine
- Gemcitabine
- Vinorelbine
- Cyclophosphamide
- Carboplatin/ cisplatin
- Eribulin
- The following combinations of chemotherapy drugs may be used for advanced breast cancer:
- FAC – cyclophosphamide, doxorubicin and 5-fluorouracil
- FEC – cyclophosphamide, epirubicin and 5-fluorouracil
- AC – doxorubicin and cyclophosphamide
- EC – epirubicin and cyclophosphamide
- Docetaxel and capecitabine
- Gemcitabine and paclitaxel
- Gemcitabine and carboplatin
- Vinorelbine and carboplatin
- Side effects of chemotherapy will depend on the type of drug, the combinations, the dose, how it is given and the patient’s overall health. Some common side effects of chemotherapy are:
- low blood cell counts
- infection
- nausea and vomiting
- sore mouth and throat
- hair loss
- diarrhea
- constipation
- fatigue
- loss of appetite
- treatment-induced menopause
- cognitive changes
- nervous system damage
- fertility problems
Immunotherapy
- Immunotherapy is designed to boost the body's natural defences to fight the cancer. The most commonly used immunotherapy for breast cancer is immune checkpoint inhibitors.
- Examples of immunotherapy: Pembrolizumab, Dostarlimab
- Administration: given intravenously every 3 or 6 weeks
- Pembrolizumab
- A combination of pembrolizumab with chemotherapy (albumin-bound paclitaxel, or paclitaxel, or gemcitabine plus carboplatin) for patients with locoregional recurrent unresectable or metastatic triple-negative breast cancer whose tumours express PD-L1 (CPS ≥10).
- Compared with chemotherapy alone, adding pembrolizumab on top of chemotherapy improved the progression-free survival in patients with advanced triple-negative breast cancer whose tumours express PD-L1 (CPS ≥ 10).
- Dostarlimab
- A type of immunotherapy for recurrent unresectable or metastatic breast cancers that have DNA mismatch repair deficiency (dMMR) or microsatellite instability-high (MSI-H) and have progressed on previous treatment.
- Side effects:
- One big concern about immune checkpoint inhibitor medicines is that they may allow the immune system to attack healthy cells and organs. As the medicines essentially take the brakes off the immune system, T cells may start attacking cells other than cancer cells. Some serious side effects include problems with the lungs, liver, intestines, pancreas, and kidneys.
Targeted therapy
- Sacituzumab govitecan
- For treatments of patients with metastatic triple-negative breast cancer who have already received at least one prior treatment for metastatic disease.
- Sacituzumab govitecan is an ADC, whereas the antibody attaches to a cancer cell then delivers the anticancer drug it carries to disintegrate the cancer cell.
- Administration: given intravenously, on days 1 and 8 of every 21-day cycle.
- Common side effects: neutropenia, diarrhea, nausea and vomiting, and allergic reaction.
Others
For patients with BRCA1 or BRCA2 gene mutation
- For patients with metastatic, HER2-negative breast cancer who have a BRCA1 or BRCA2 gene mutation, oral PARP inhibitor may be an option.
- Olaparib/ Talazoparib
- Administration: oral medication, taken twice or once a day
- Olaparib and talazoparib belong to PARP inhibitors which destroy cancer cells by preventing them from fixing damage.
- Common side effects: fatigue, nausea and vomiting, headaches, diarrhea, decreased appetite, hair loss and lower levels of certain blood cells.