Palliative care is an approach that improves the quality of life of patients (adults and children) and their families who are facing life-threatening illness. It prevents and relieves suffering through early identification, correct assessment and treatment of pain and other pain and other symtoms, whether physical, psychosocial or spiritual. Palliative care affirms life and regards dying as a normal process. It neither hastens nor postpones death. Palliative care is a holistic approach that involves a multidisciplinary team. It offers a support system to help patients live as active as possible until a death. Moreover, it offers a support system to the families to cope during the patient’s illnesses and in their own bereavement.

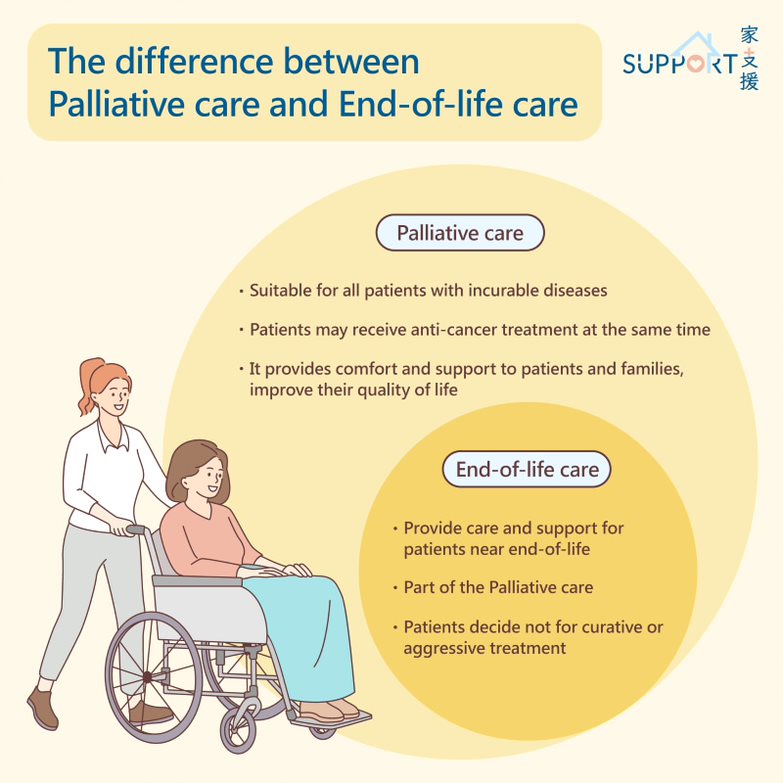
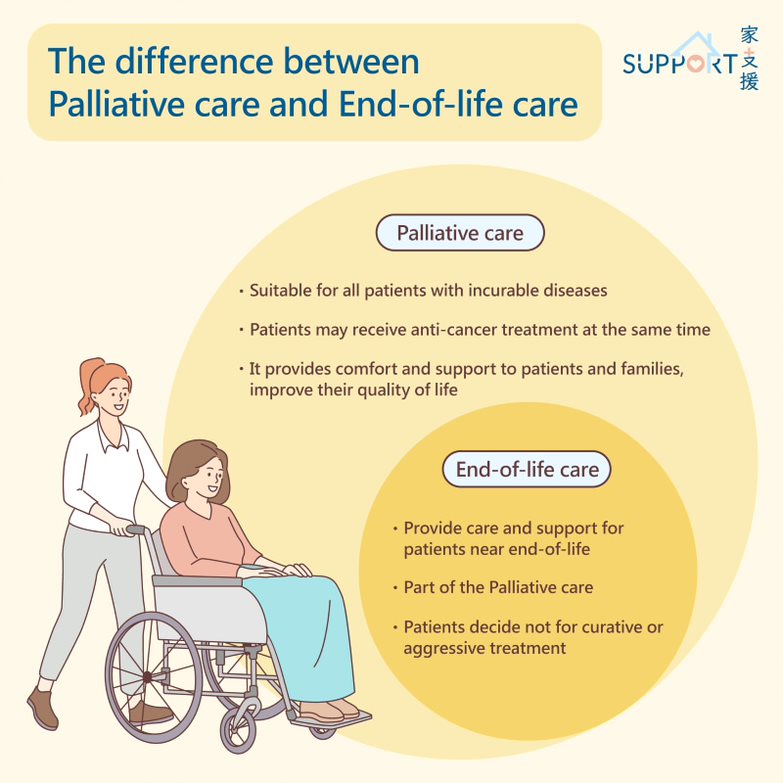
Palliative Care and End-of-life care
|
Palliative Care
- Palliative care is the management plan to care and support patients with life-threatening illness and their families.
- Patients on palliative care may still receive treatment for their diseases, e.g. chemotherapy or targeted agents.
- Goal: provide comfort, quality of life, support to patients and families
|
|
End-of-life care
- End of life care involves treatment, care and support for people who are nearing their end of life.
- End-of-life care is a part of the palliative care.
- Life expectancy is usually less than 6 months.
- Patients at end-of-life have chosen not for curative or aggressive treatment.
- Goal: provide comfort to patients and family
|
The multidisciplinary team
Below are the people in the multidisciplinary palliative care team:
- Palliative care doctor
- Oncologists
- Nurses
- Pharmacists
- Social workers
- Physiotherapists
- Occupational therapists
- Counsellors/ Spiritual counsellors
- Volunteers
Services of palliative care
- Providing support to patients and families
- Providing physical, psychological, social and spiritual care
- Providing grief and bereavement support
- Social workers, financial counselling and caregiver training
- Advanced care planning
- Home care, day care, consultation services and hospice inpatient care
All patients with life-threatening illnesses benefit from palliative care, such as:
- advanced cancer
- end-stage kidney, heart, lung, liver and neurological diseases
- frailty related illness such as advanced dementia, Parkinson’s disease
Locations of receiving palliative care
- Patients’ homes
- Nursing homes
- Hospices
- Specialist clinics
- General and community hospitals
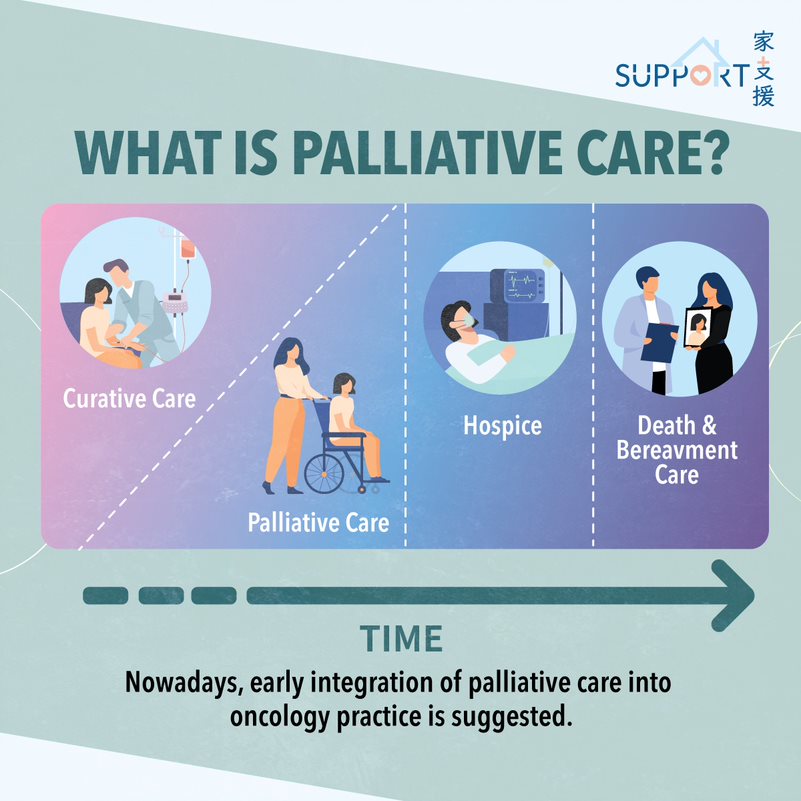
Timing for palliative care
In the past, palliative care was started only after all anti-cancer treatment is exhausted.
- Problems include:
- Persistent, unattended symptoms and distress in the phase of active treatment
- Patients and families feeling “abrupt” referral to palliative care service and felt abandoned by their mother team – oncologists.
- Patients and families having less time to prepare for the deterioration.

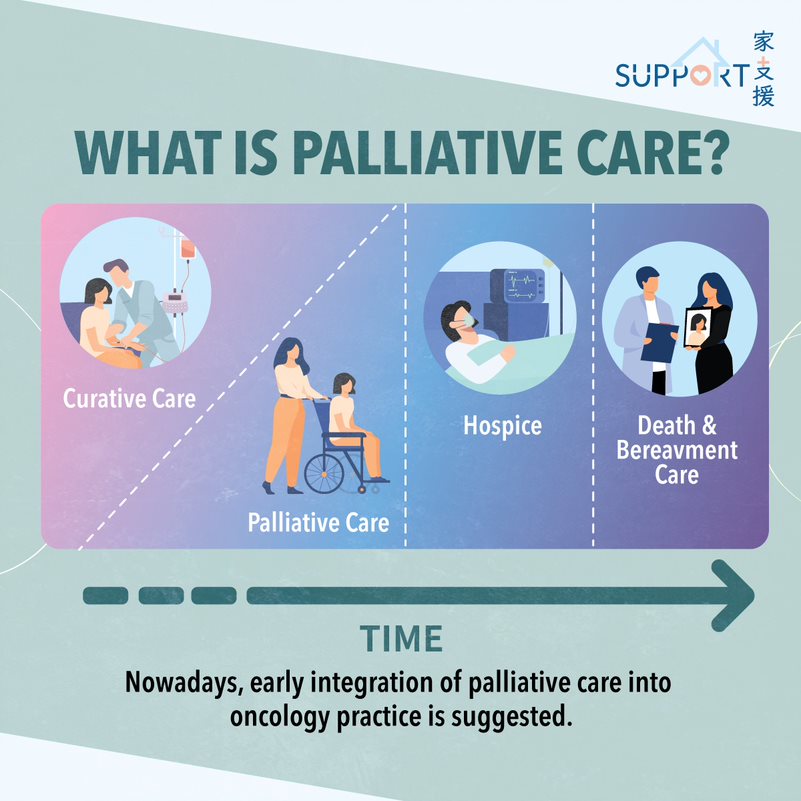
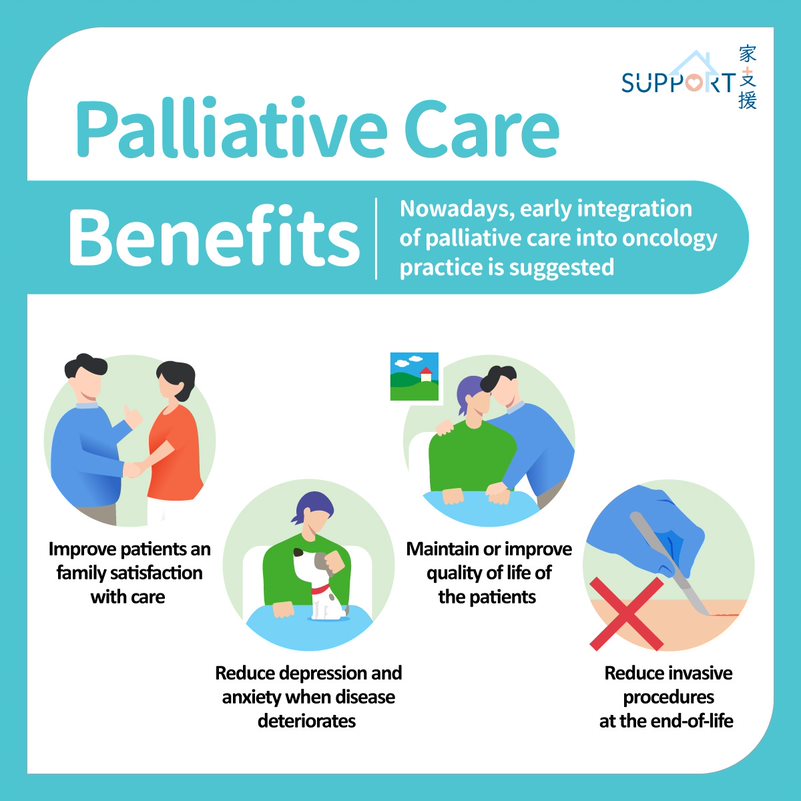
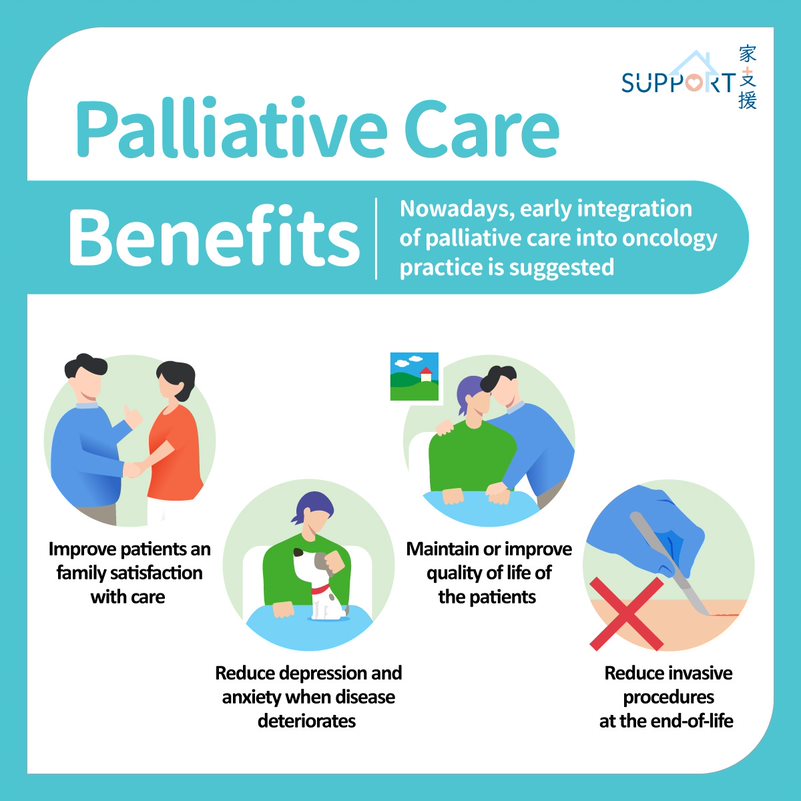
Nowadays, early integration of palliative care into oncology practice is suggested. Its benefits include:
- Improving patient’s and their family’s satisfaction with care
- Maintaining or improving quality of life of the patients
- Preventing depression and anxiety when disease deteriorates
- Reducing invasive procedures at the end-of-life
Videos
▶️ Palliative Care - The performer
▶️ Palliative care - Walking together