Below are several common misconceptions that are debunked by clinical oncologists:
1. If I feel pain, does it mean it is the end of the life for me?
By Dr. William Foo, Specialist in Clinical Oncology:
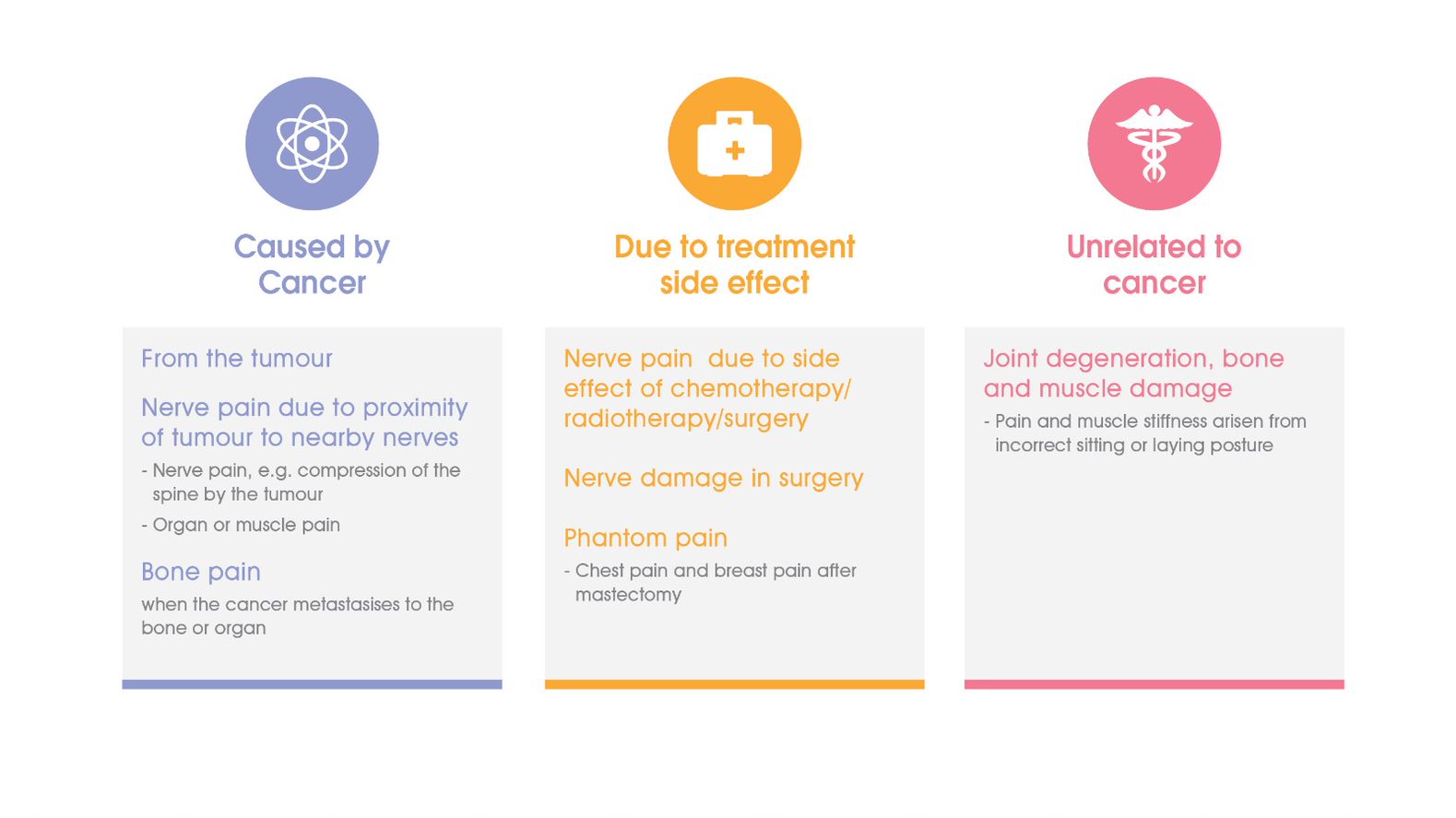
“Absolutely not! Patients will feel pain at any stage of the treatment process, and it is the most common symptom in cancer patients. Pain can be the direct result of tumours, treatment procedures such as surgeries, chemotherapy or radiotherapy, or even be completely unrelated to tumours or cancer itself. Some types of pain go away completely after a tumour has been removed. Other times, it is when the side effects from treatment wear off. However, with some forms of long-lasting pain, this can continuously affect the patient negatively. So with that said, pain doesn’t always mean that one’s condition is taking a turn for the worse.”
2. Treating cancer is the most important, which means that pain management is not, right?
By Dr. Lam Tai Chung, Specialist in Clinical Oncology:
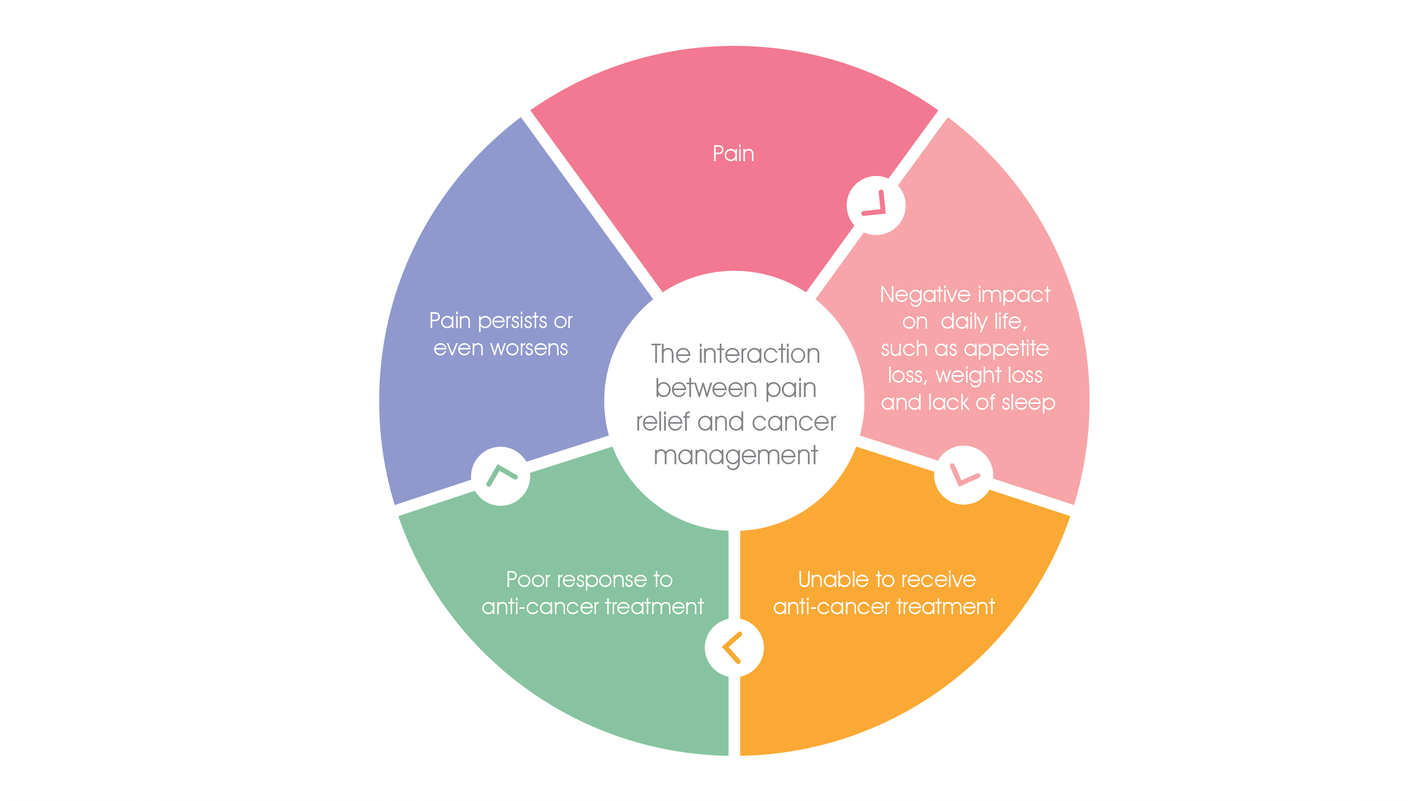
“Pain management is one of the most important factors to be considered during cancer treatment, being just as high-priority as targeting the cancer itself. The sooner patients proactively seek treatment, the sooner the pain and any discomfort will be effectively managed. This has direct consequences to patients’ survival outlook, quality of life and mental health.”
3. Since I cannot avoid pain, so will simply enduring it do me any good?
By Dr. Chan Po Chung, Specialist in Clinical Oncology:
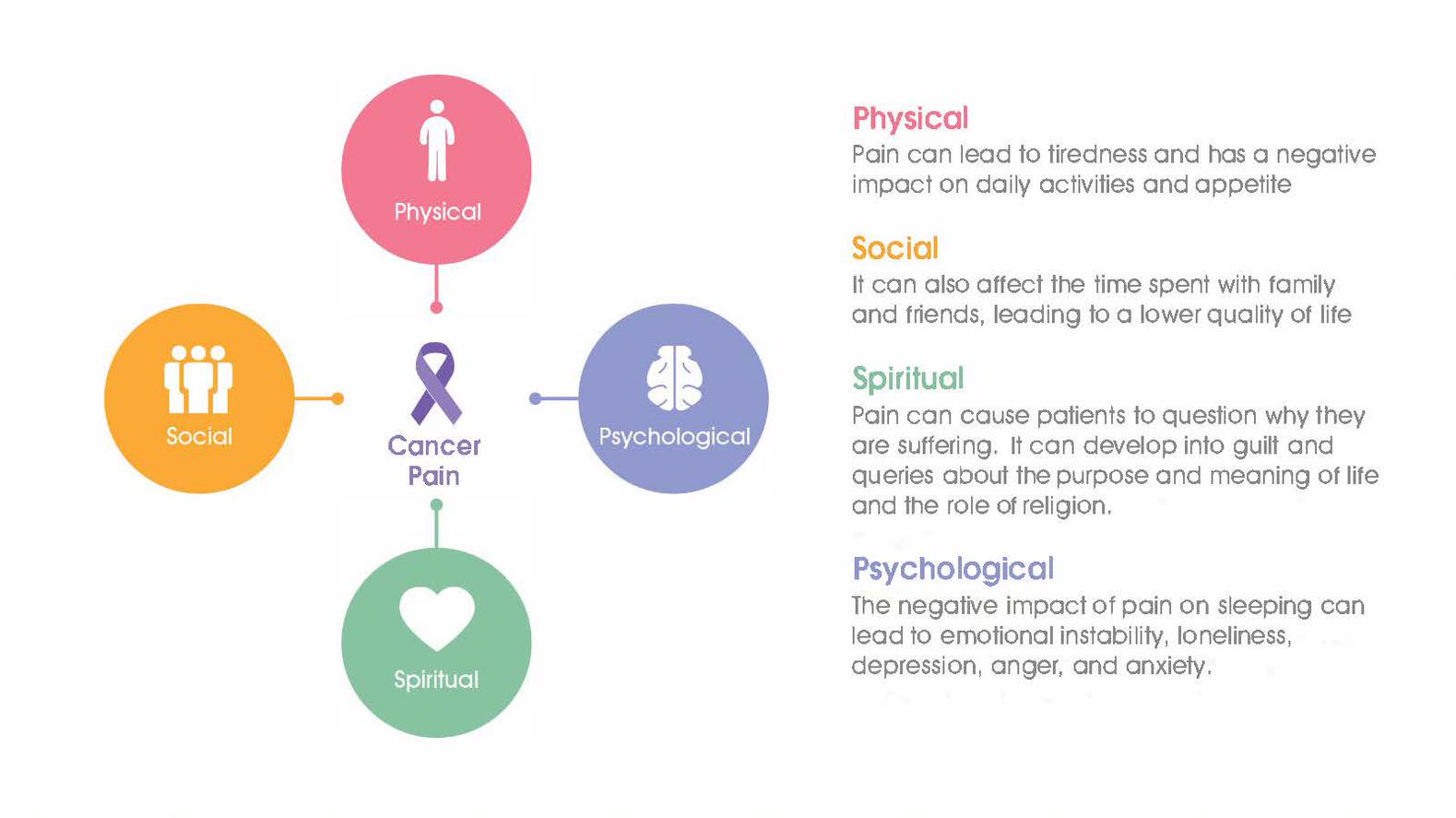
“Endurance is considered a virtue in traditional Chinese philosophy. However, this alone does not apply to cancer patients, as it will not take them very far. In fact, there is just no need in suffering excruciating pain. Inadequate pain management will have far-reaching effects on the patient’s sleep, appetite, as well as mental and physical health. The consequences could even extend to stopping cancer treatment. Taking painkillers at the right time not only makes the patient feel better, but also allows them to maintain a good quality of life. In the long run, this could equate to effective control of the cancer itself.”
4. Should I wait until there’s pain or when it gets unbearable before taking my medication?
By Dr. Macy Tong, Specialist in Clinical Oncology:
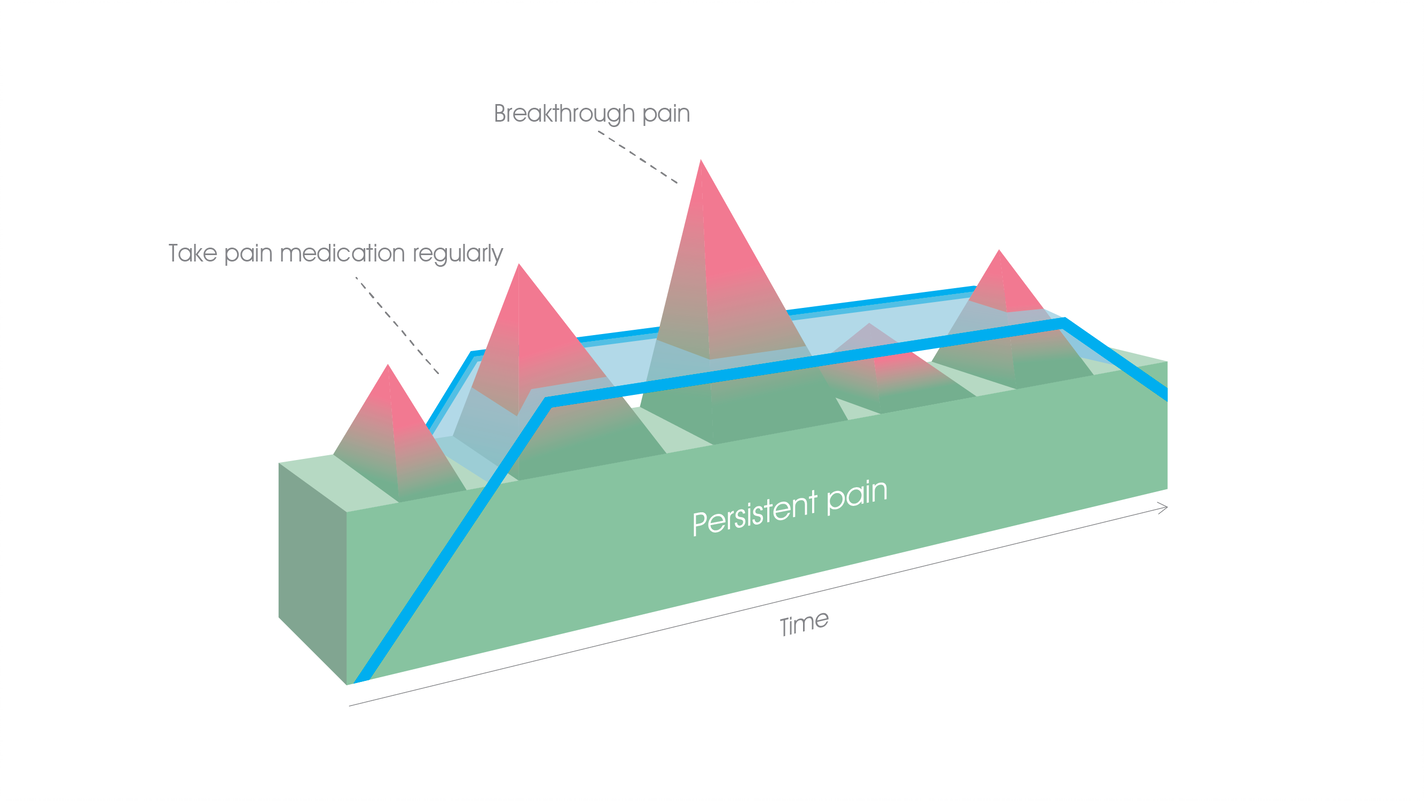
“The key tenet of pain management during cancer treatment is, “Solving the problem before it even happens”. Waiting until it becomes unbearable is never the right way to manage pain properly. Taking medication in a hurry just as pain sets in reduces its overall effectiveness, leading to a common misconception that the painkillers do not work at all. In fact, doing so will actually drastically increase the risk of additional side effects.”
5. When the painkillers are not alleviating my pain, they will not work anymore, right?
By Dr. Carmen Leung, Specialist in Clinical Oncology:
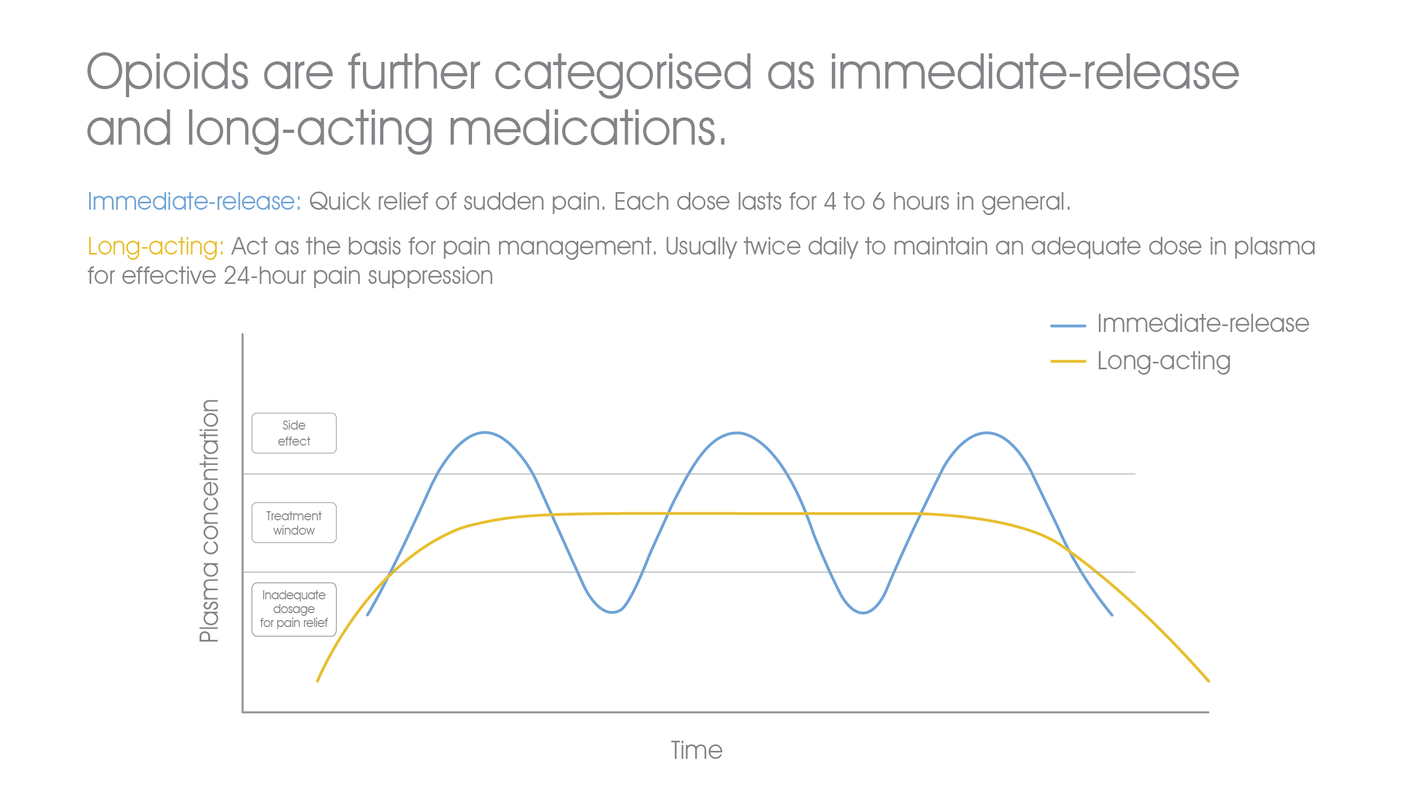
“It is a very common misconception among patients. When painkillers are prescribed properly, there is very little chance that the medication is ineffective. Patients are usually misguided after seeing just the first dose or two not delivering the desired effect, losing confidence in their prescriptions. It is noteworthy that medicines never come into effect the moment they are swallowed. However, taking long-acting medication has been proven to prevent slow reactions to painkillers.”
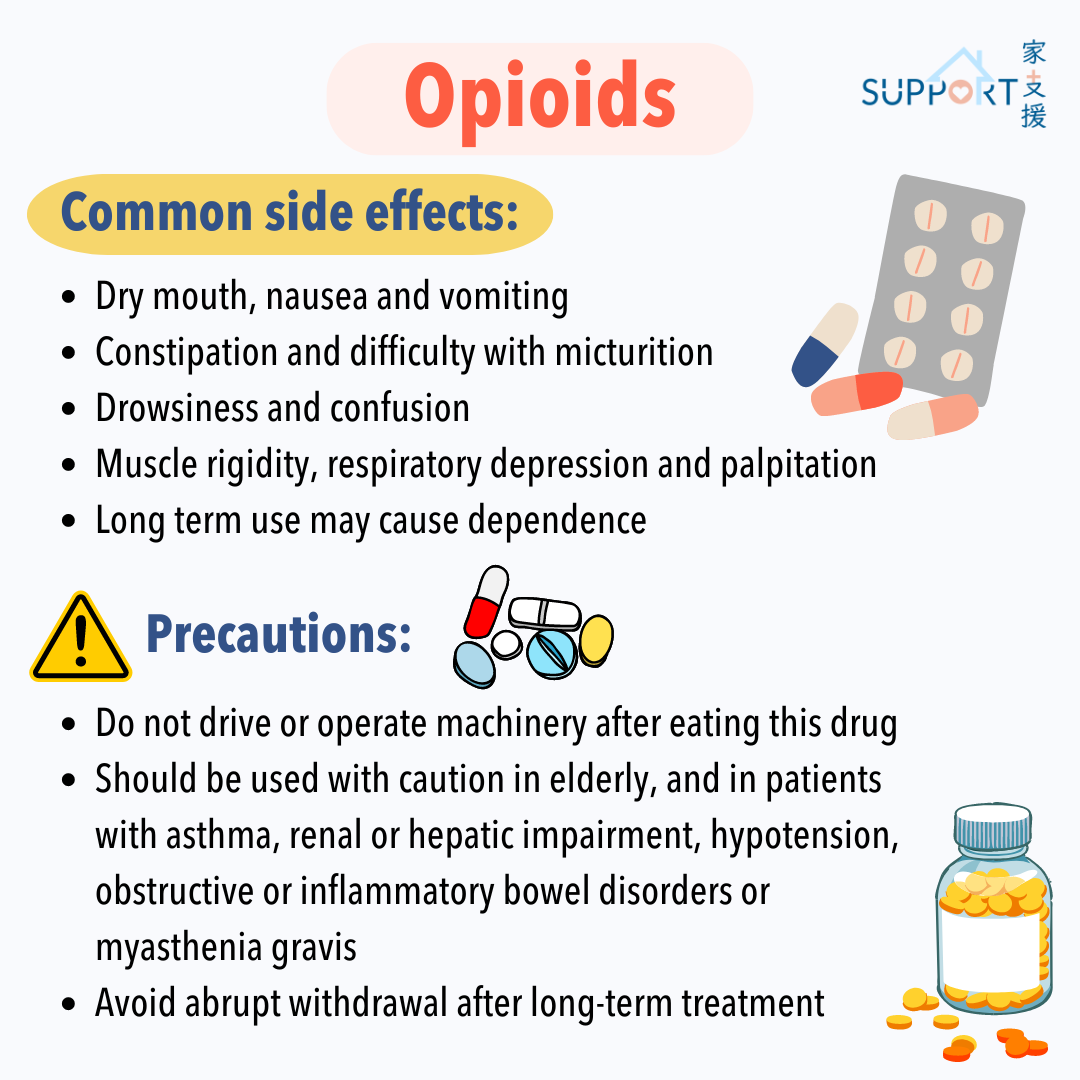
6. Painkillers pose many side effects. Will there be a 100% chance of addiction?
By Dr. Lim Mei-ying, Specialist in Clinical Oncology:
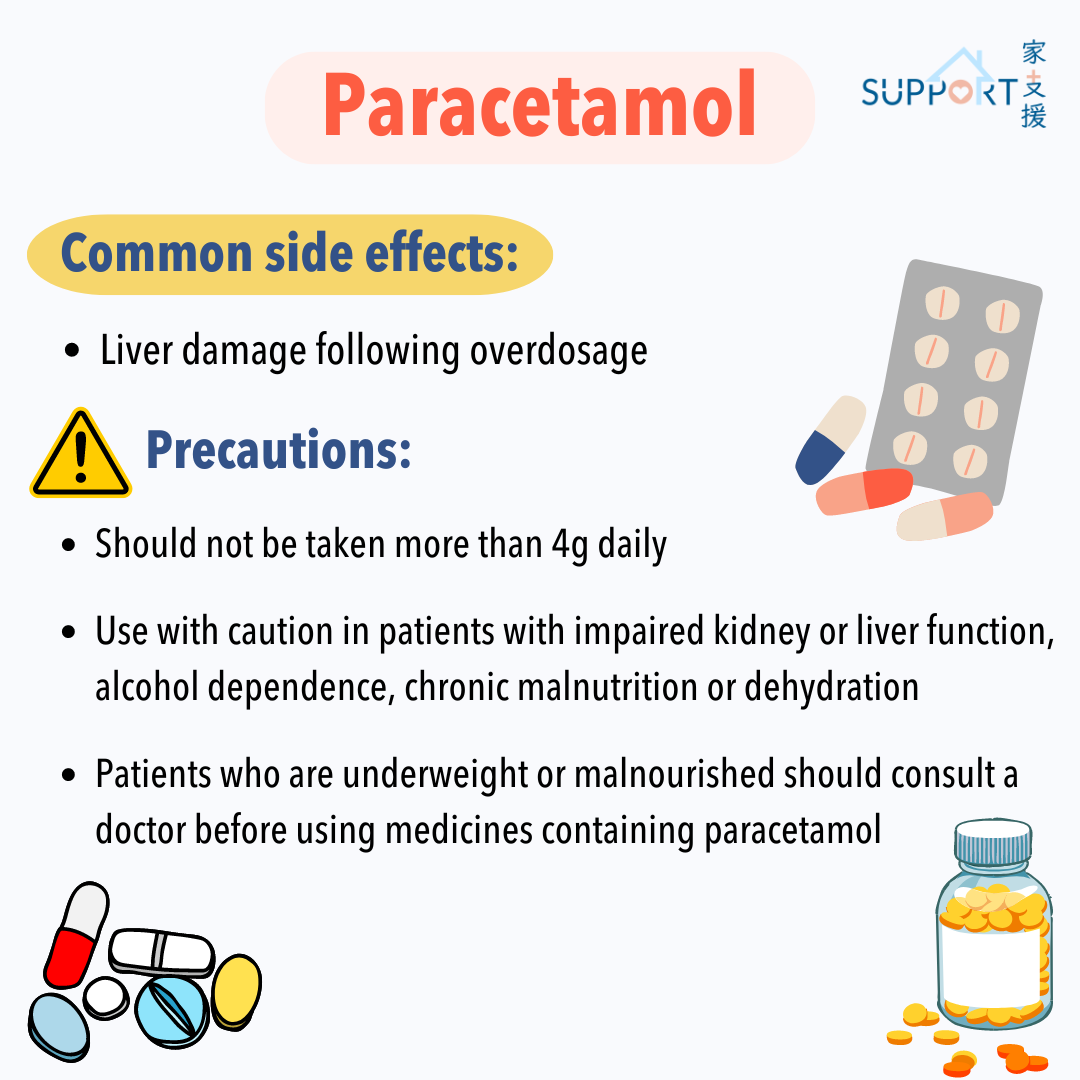
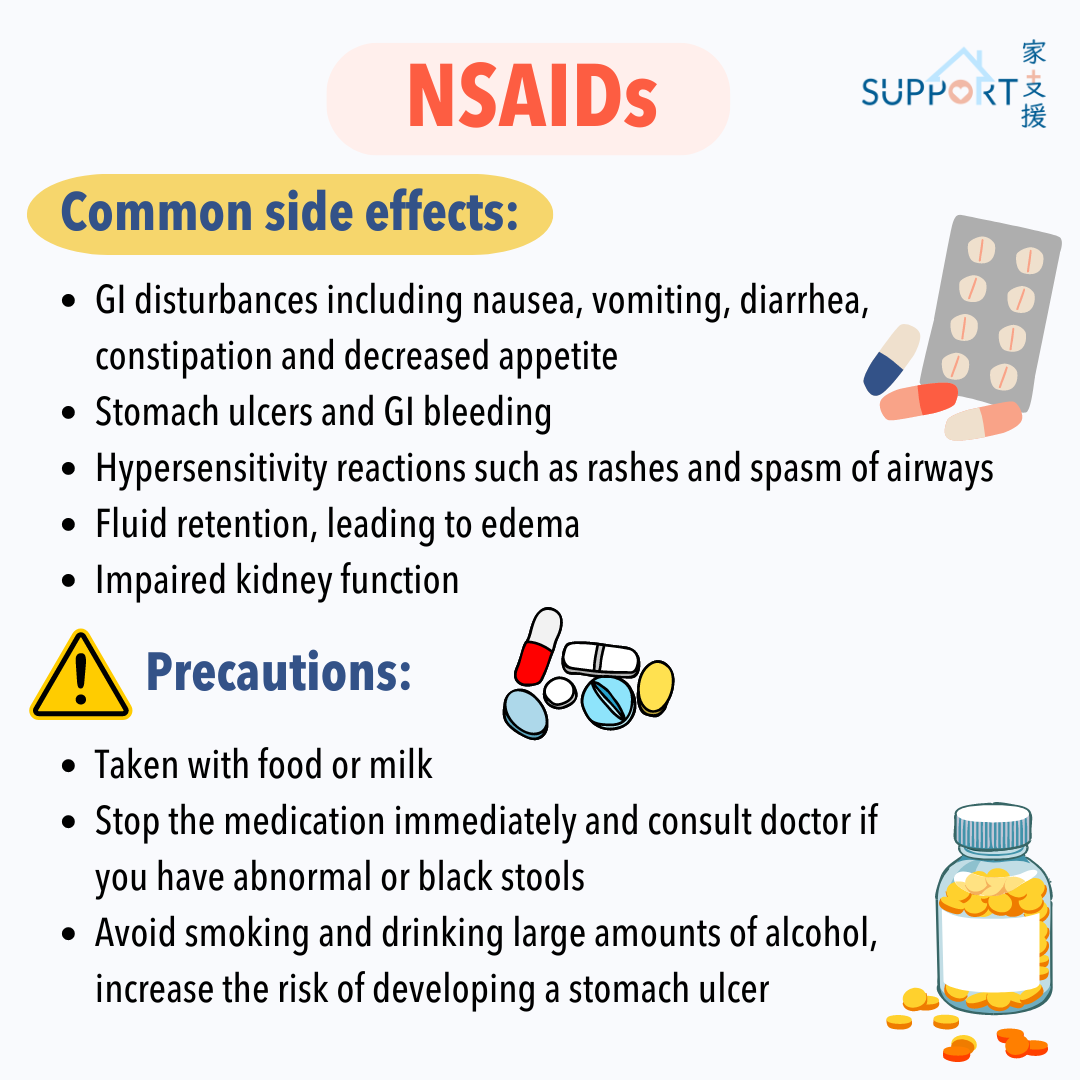
"Every medication has side effects. Those of painkillers normally include tiredness, nausea, a stuffy nose, vomiting and constipation. Most of these are mild and commonly observed, so doctors can prescribe other drugs in advance to prevent them. If the patient is too responsive to side effects, the doctor can also switch to a new type of painkiller to reduce them. As seen in daily clinical practice, there are actually more cases of self-discontinuation on the part of the patient than doctors asking patients to discontinue medication. Addiction should not be a primary concern at all as every medication is tailor-prescribed to prevent this from happening.”
7. Will discussing pain with my doctor prevent them from concentrating on my cancer treatment?
By Dr Inda Sung Soong, Specialist in Clinical Oncology:
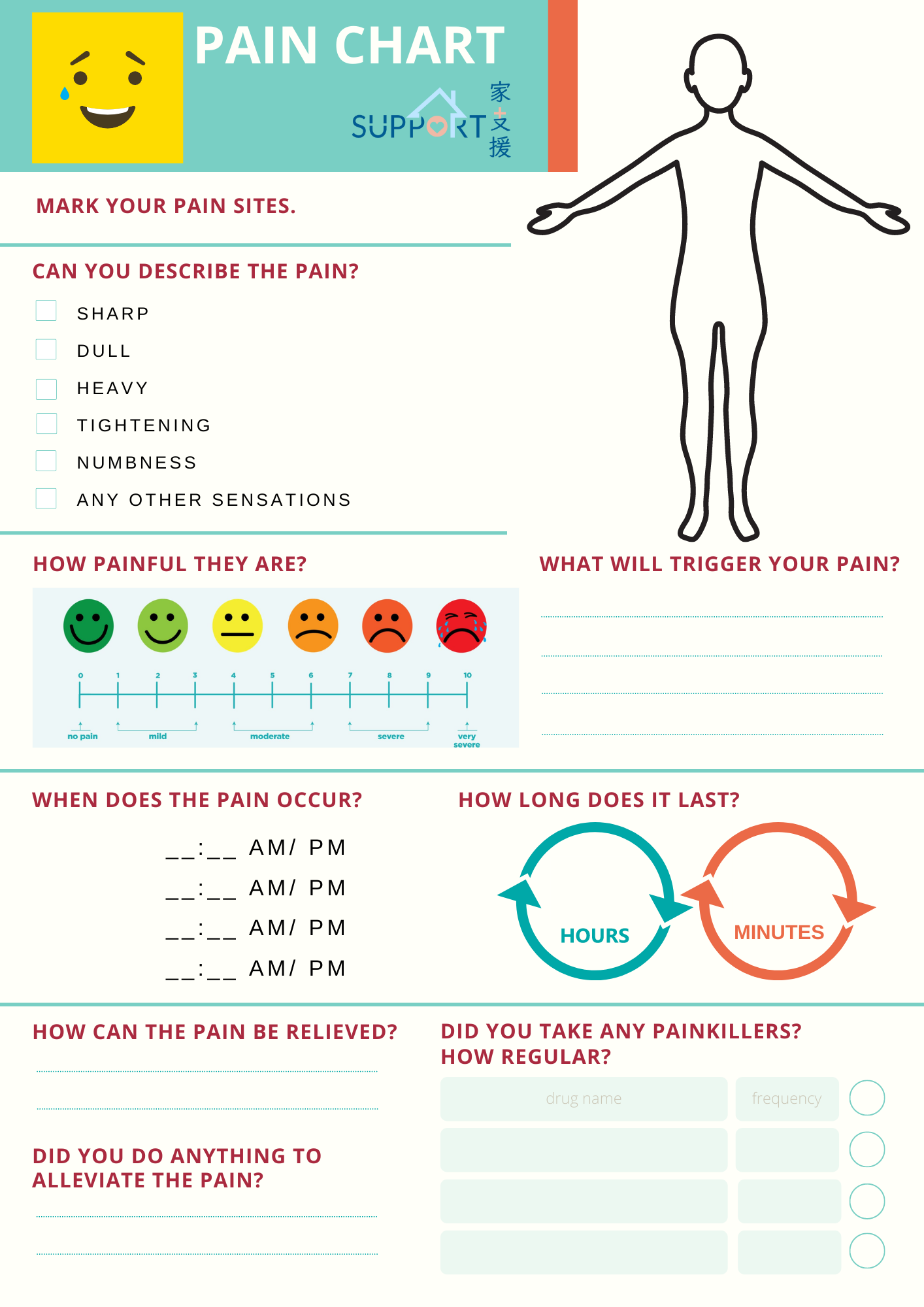
“Us oncologists invest a great deal of attention on pain management. Patients are more than welcome to take the initiative to discuss any instance of pain with their doctor. Therefore, patients can take the initiative to share their views and perceptions of pain with the doctor. Small details such as pain intensity and situation, when and where the pain occurs as well as its impact on life can potentially be life-changing. This information will help doctors understand the extent of the pain and develop appropriate methods for relieving the pain. In addition to medication and interventional treatment options, some hospitals also provide psychological assistance and spiritual support to patients, providing a comprehensive approach to pain relief for them.”
8. I want to be as transparent as possible to my doctors and health professionals. How should I organise information for discussions about my pain?
As should be known, simply relying on memory to recount any pain you’ve suffered between check-ups is no easy task. Keeping a daily record of it allows health professionals in your support network to be updated as much as possible about your condition.