How to manage malignant biliary obstruction?
Methods to relieve the jaundice depends on the cause of obstruction of the biliary tract. Surgery or stent insertion can be used to relieve the obstruction.
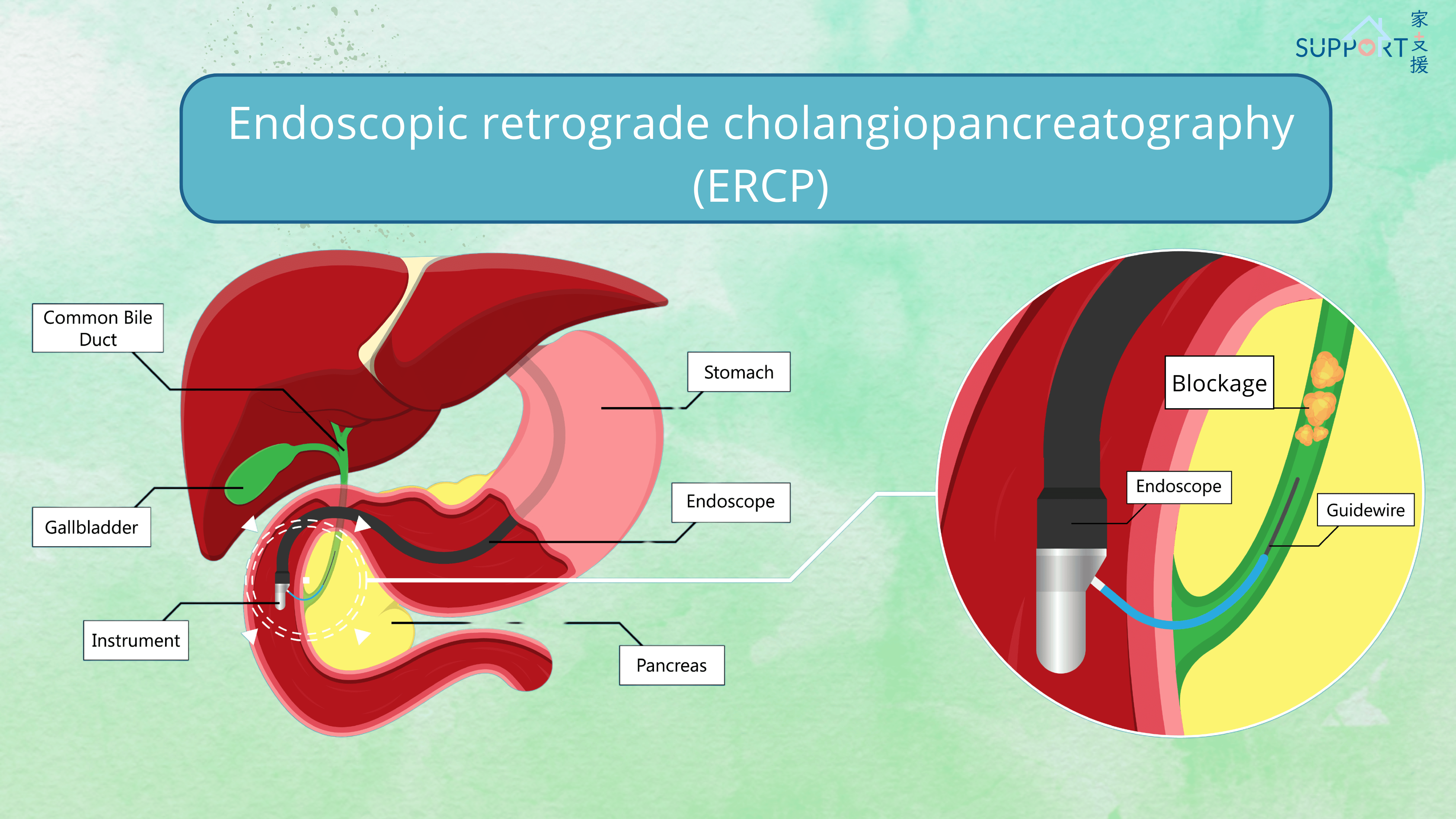
1. Endoscopic retrograde cholangiopancreatography (ERCP) and stent
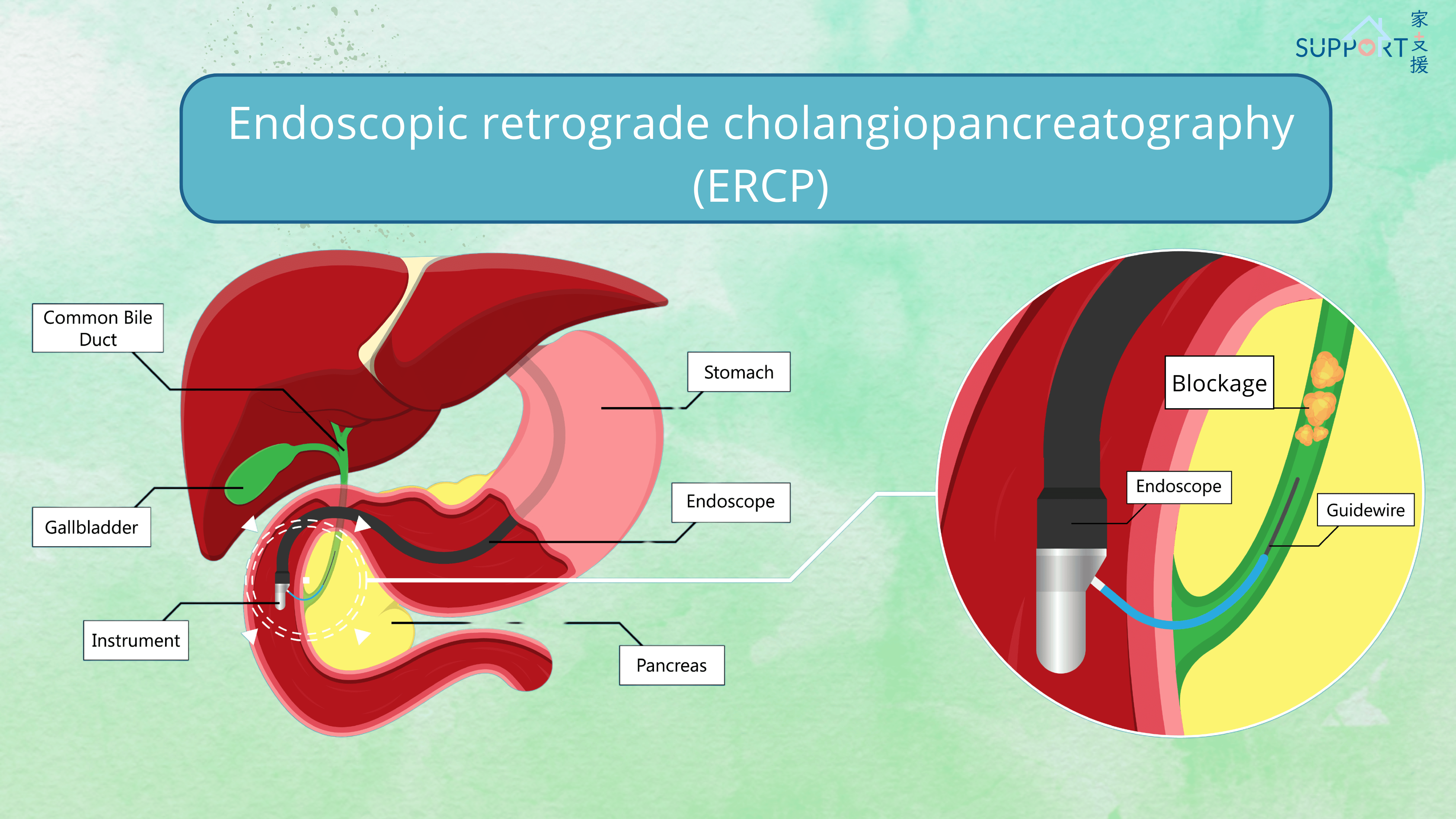
- ERCP is the gold standard of imaging of the biliary tract and can serve as both diagnostic and therapeutic purpose.
- Your doctor will put an endoscope which is a flexible tube with a camera into your mouth and pass into the duodenum for access to the bile duct. A smaller scope is then advanced into the bile duct. Dye is injected into the bile ducts and X-rays are taken to the locate the site of obstruction.
- Biopsy is usually taken during the procedure to get a pathology to confirm the diagnosis.
- A stent, either plastic or metallic, can be inserted at the site of blockage to allow the bile to drain into the intestine again. You will usually notice a benefit within 1-2 days after stent insertion.
- The procedure is performed under anaesthesia and requires pre-operative fasting for 6-8 hours. Antibiotics is injected before the procedure to lower the risk of infection.
- Risk of ERCP: biliary contamination (bacteria from the intestines enter the biliary system), pancreatitis, bleeding, allergic reaction to the anaesthetic agent or contrast dye, small bowel perforation, stent occlusion
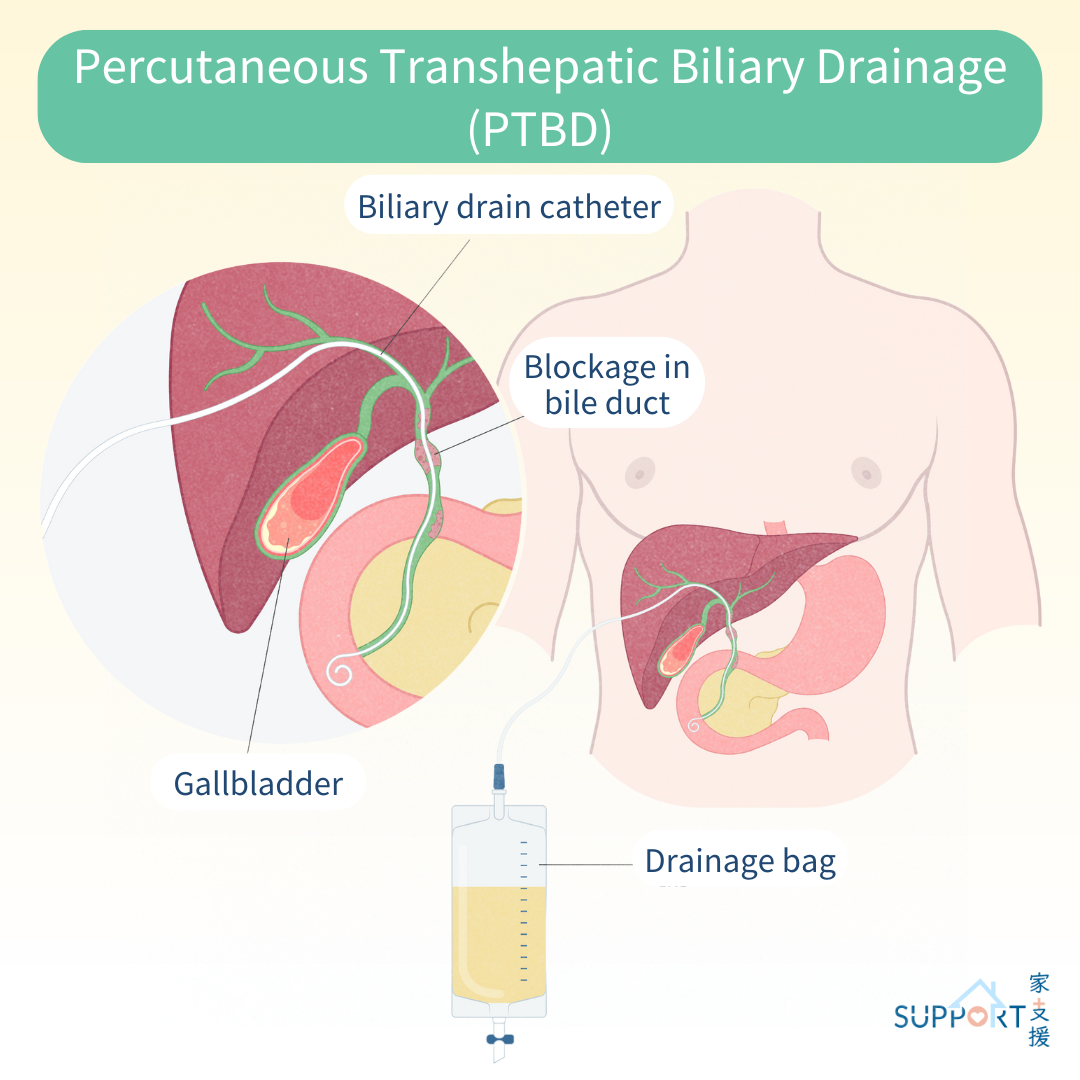
2. Percutaneous transhepatic cholangiography (PTBD)
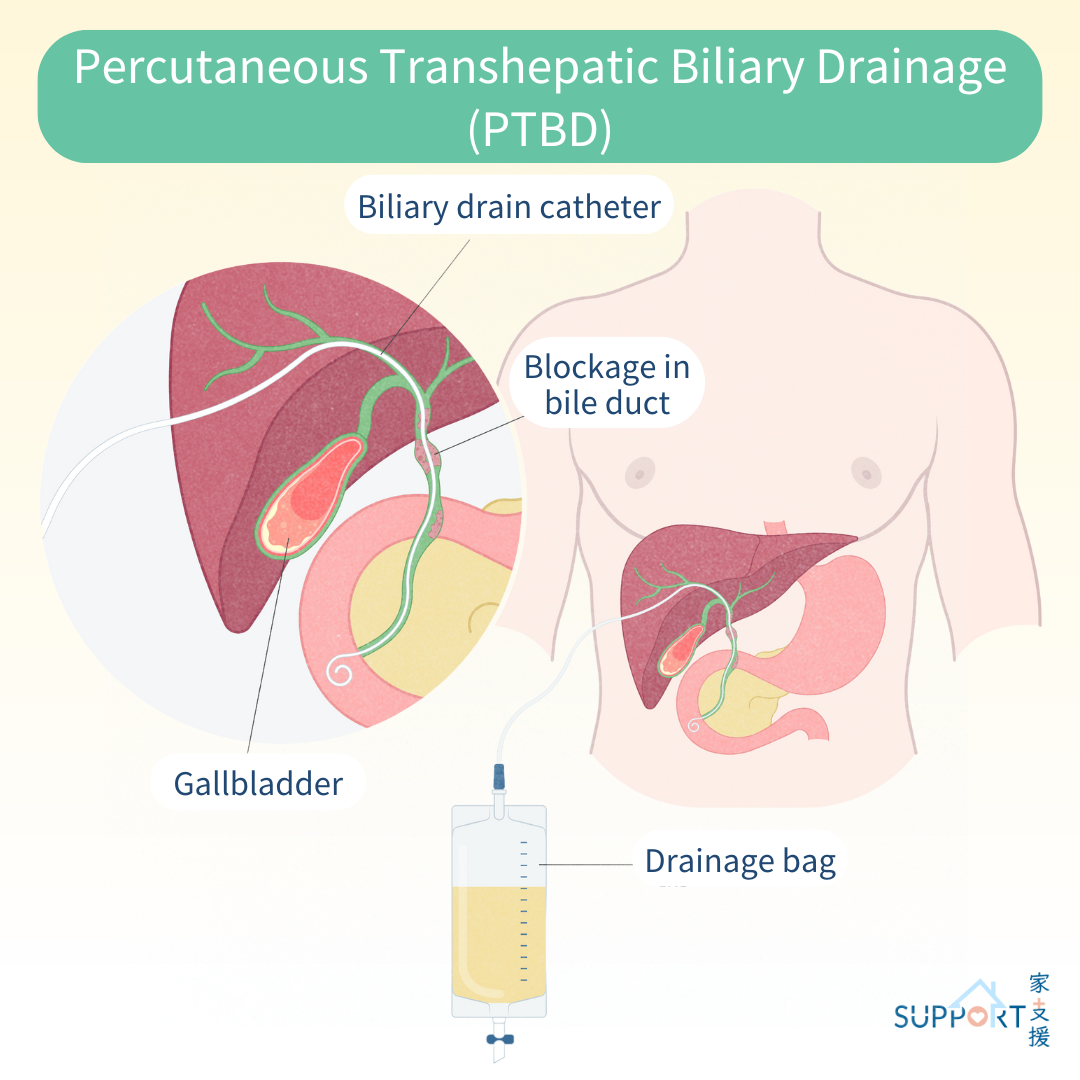
- PTBD is performed if ERCP is unsuccessful or unavailable. It is a minimally invasive procedure where a thin tube called a catheter is inserted into the liver through a skin puncture. One end of the tube enters the bile duct, while the other remains outside the body. The bile is drained and collected in a bag outside your body.
- This procedure is performed under local anaesthesia. Guided by ultrasound, a needle is inserted into the bile ducts within the liver. A contrast dye is then injected to visualise the biliary tree with X-Ray. A guidewire is then advanced past the area of obstruction at the biliary tract and a catheter is placed to drain the bile out.
- Risks: bleeding, bile leakage, catheter dislodgement or blockage, infection due to skin penetration and indwelling foreign body, severe infection due to liver puncture, accidental puncturing of neighbouring organs such as arteries, lungs or bowels, contrast dye allergy.
3. Bypass surgery
- If the patient is fit enough, a surgical procedure called biliary bypass may be an option of relieve the obstruction. Your doctor may perform a bypass surgery that connects the part of bile duct before and past the obstruction sites. For example, a bypass surgery that joins the common bile duct to the jejunum or a surgery that joins the biliary duct from the liver to the jejunum.
- The surgery can be done by opening the abdomen or by keyhole surgery.
4. Radical operation
- If the cancer is localised, your surgeon will discuss your case with oncologist and radiologist in multidisciplinary tumour board meeting to determine if radical surgery can be performed.
- However, usually the jaundice needs to be relieved with lowering down of the serum bilirubin level before radical operation.
- The type of operation depends on the site and local extent of the cancer.
5. Radiotherapy
- If the tumour that causes biliary obstruction cannot be surgically removed, palliative radiotherapy can be given to relieve pain and potentially prolong the recurrence of obstruction after insertion of the stent.
- You will first undergo radiotherapy planning. The radiation therapist will make some markings on your skin at the abdomen. A CT scan will be performed. Then your oncologist will use the CT scan to delineate the site for radiotherapy and determine the radiotherapy dose.
- The duration of radiotherapy usually lasts for 2 to 5 weeks, depending on the total dosage of the radiotherapy.
- Side effects of radiotherapy: skin reaction (redness or desquamation), stomach discomfort, dyspepsia, diarrhoea, malaise
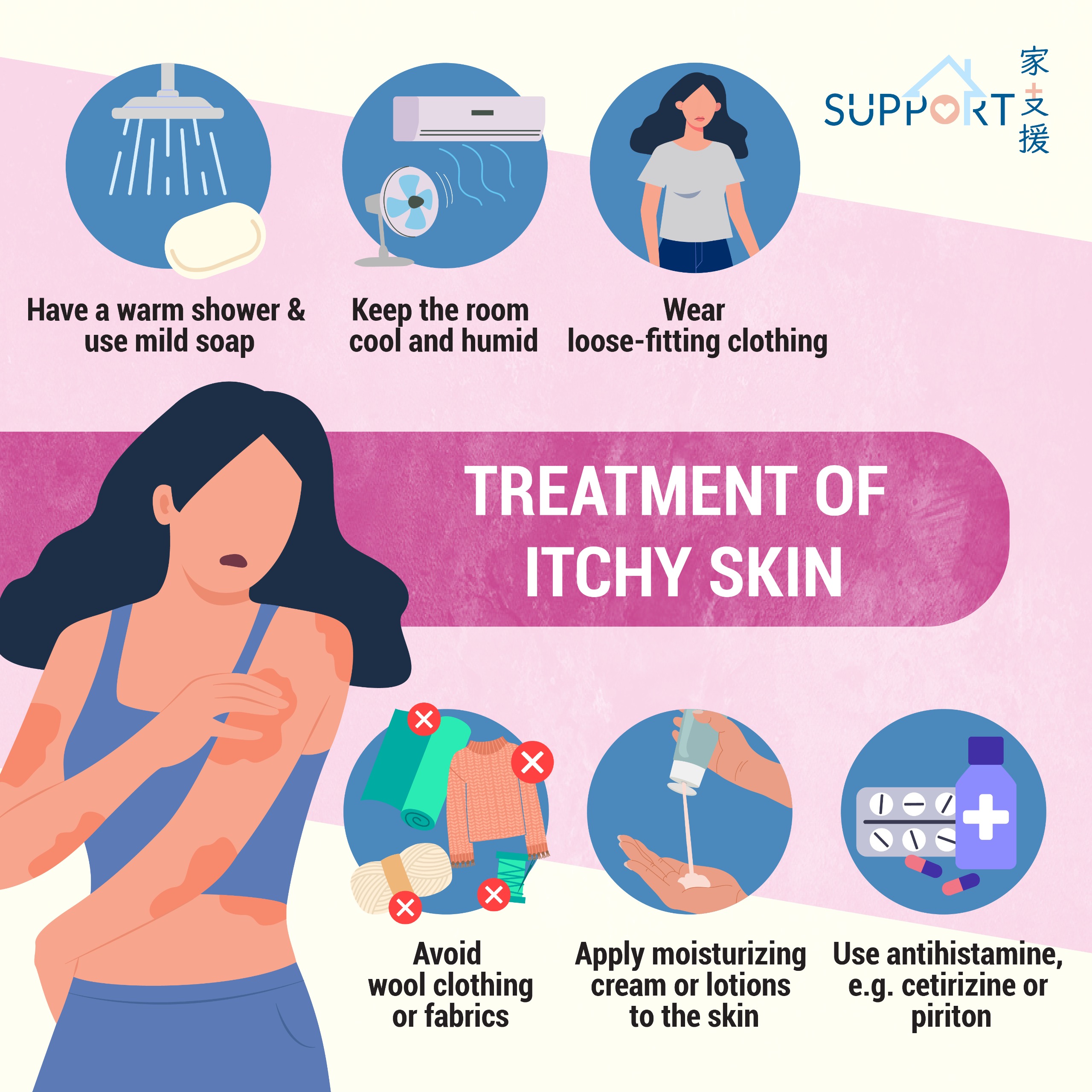
6. Treatment of itchy skin
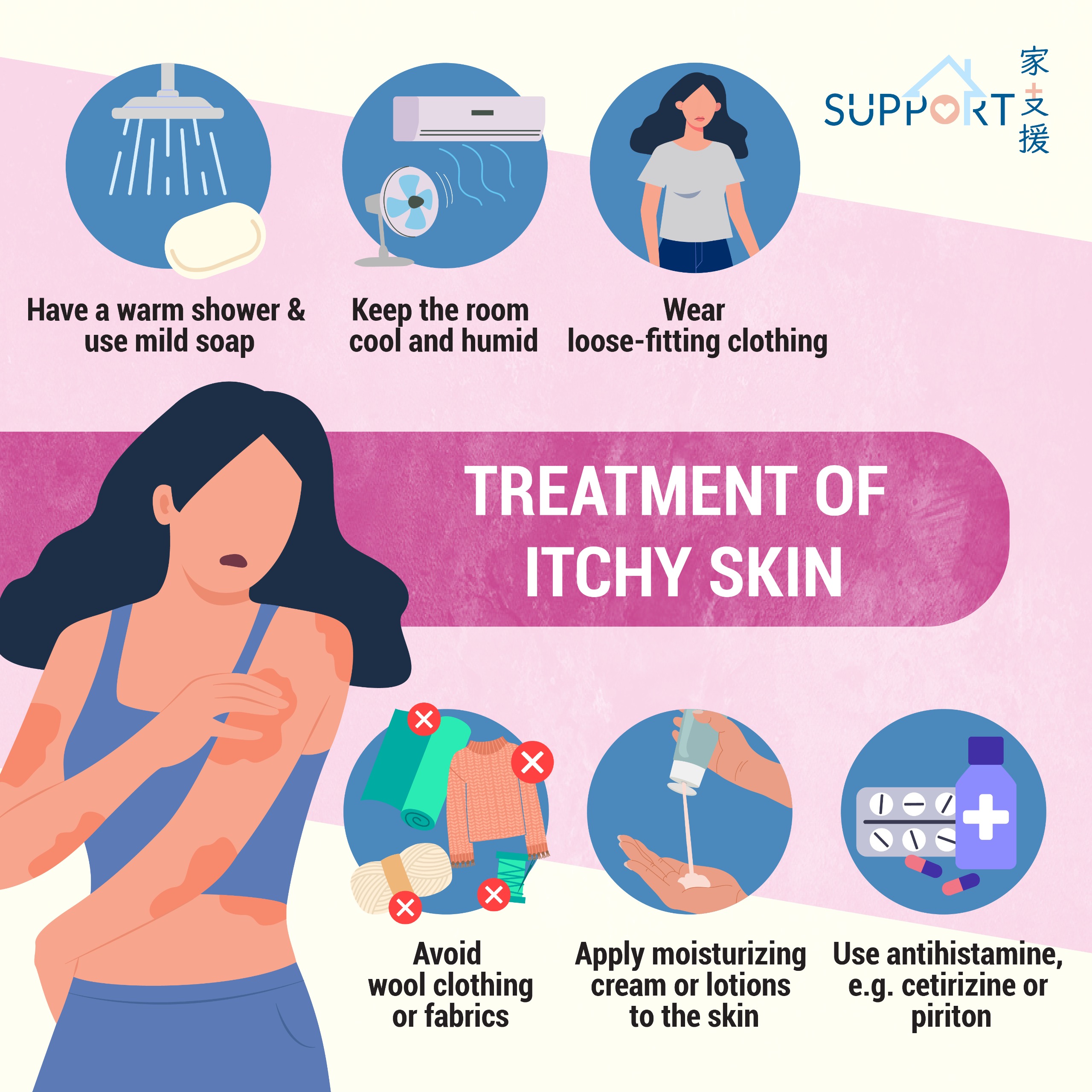
- Itchy skin results from bile salt deposition in the skin.
- General measures to improve the symptoms:
- having a warm shower and using mild soap
- applying moisturizing cream or lotions to the skin
- keeping the room cool and humid
- wearing loose-fitting clothing
- avoiding wool clothing or fabrics that irritate skin
- using antihistamine, e.g. cetirizine or piriton, to relieve the itchiness
- Your doctor may prescribe cholestyramine to lower the bile salts in your body for relieving the discomfort.