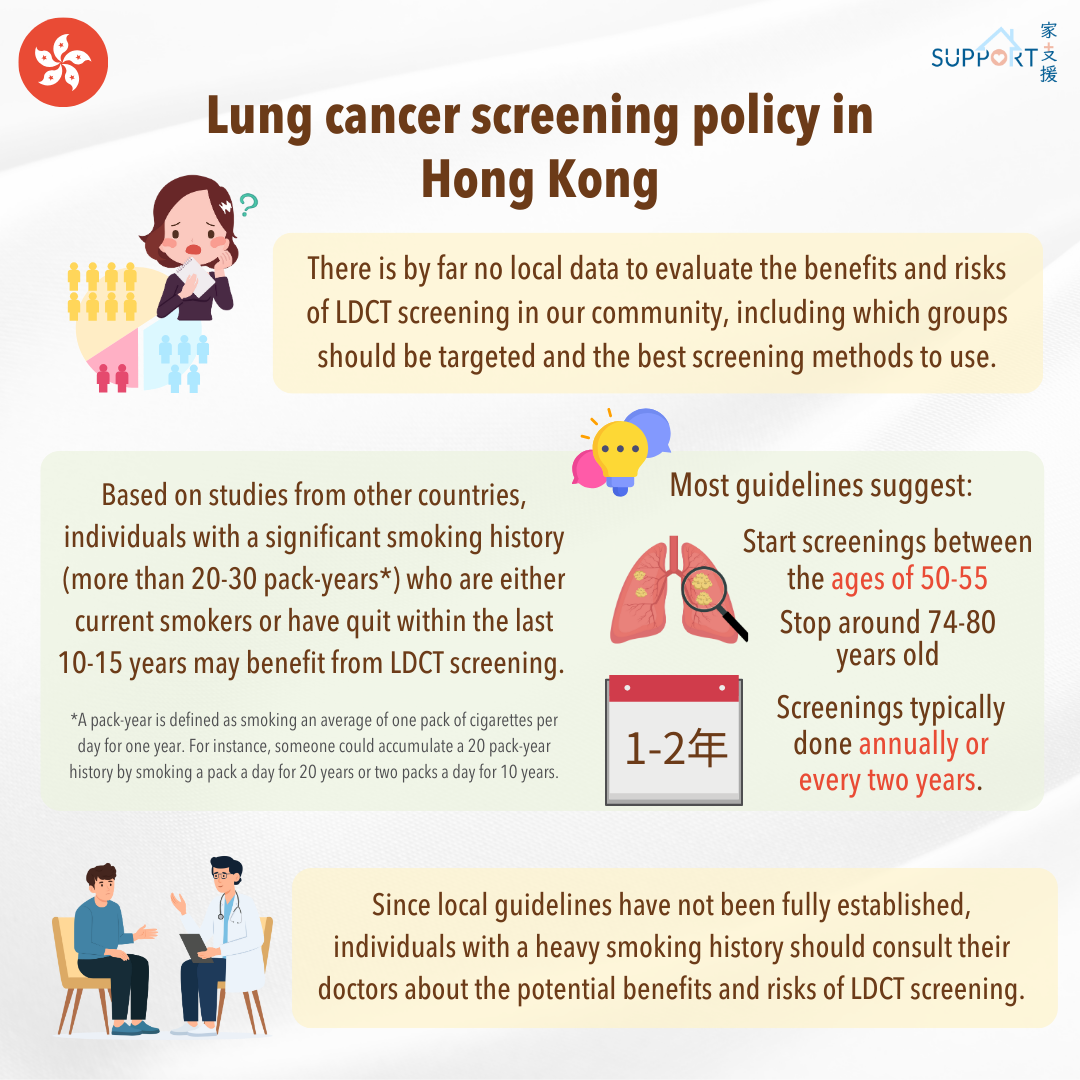
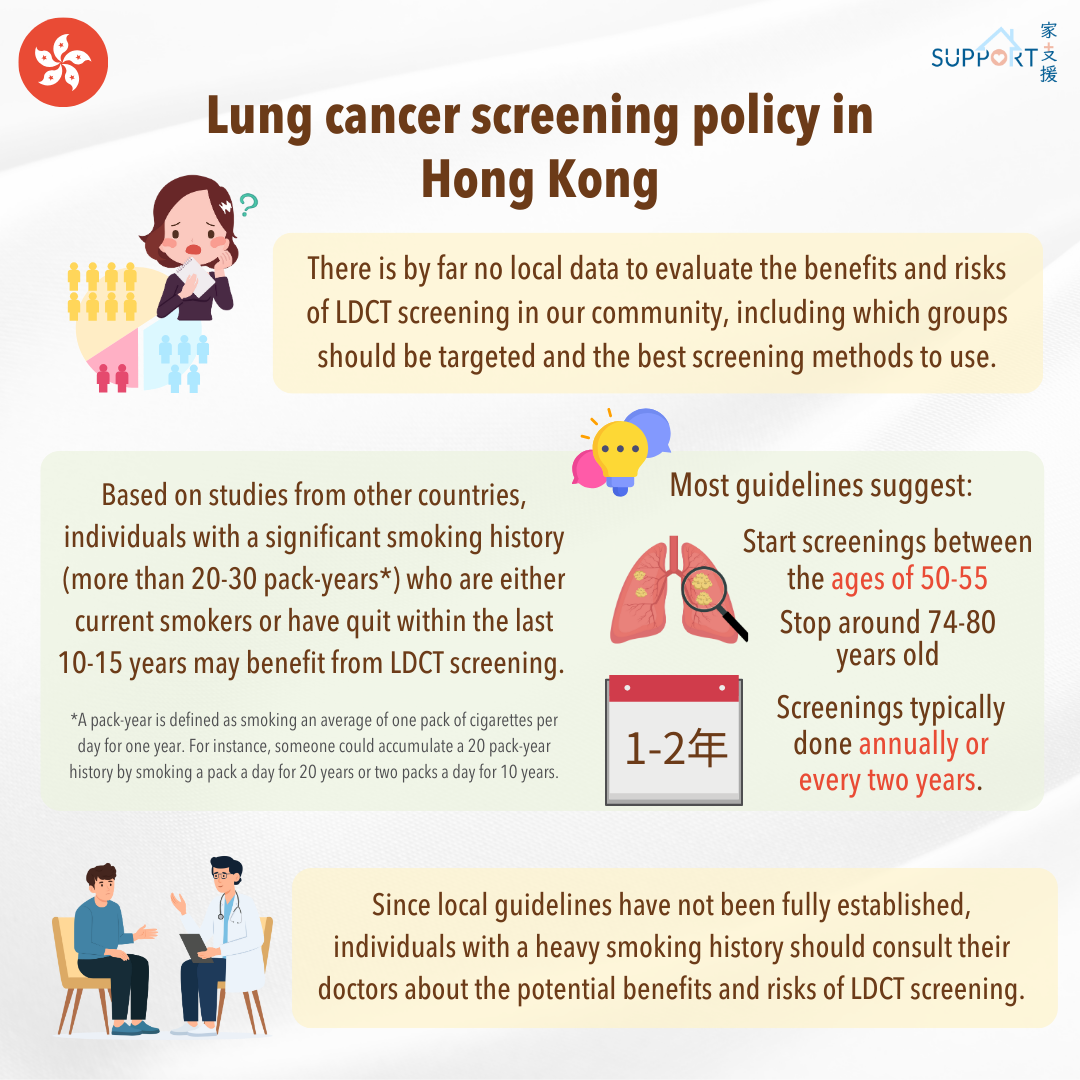
There is by far no local data to show the effectiveness of LDCT screening for individuals at high risk of lung cancer in Hong Kong. Moreover, there isn’t a validated tool to identify high-risk individuals or to establish specific guidelines for screening. Due to this lack of data, there is insufficient information to evaluate the benefits and risks of LDCT screening in our community, including which groups should be targeted and the best screening methods to use.
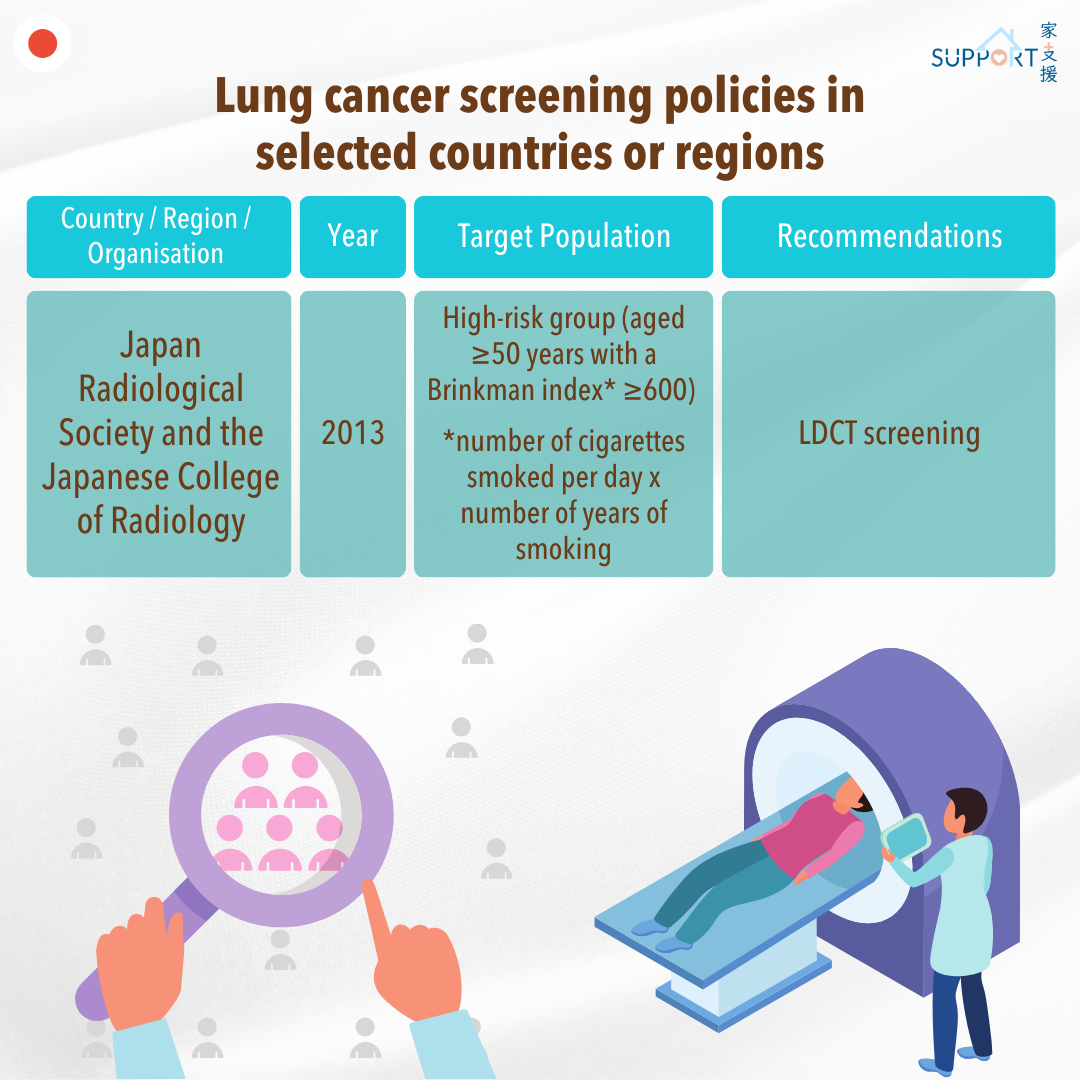
Based on studies from other countries, individuals with a significant smoking history (more than 20-30 pack-years) who are either current smokers or have quit within the last 10-15 years may benefit from LDCT screening. Most guidelines suggest starting screenings between the ages of 50-55 and stopping around 74-80 years old, with screenings typically done annually or every two years.
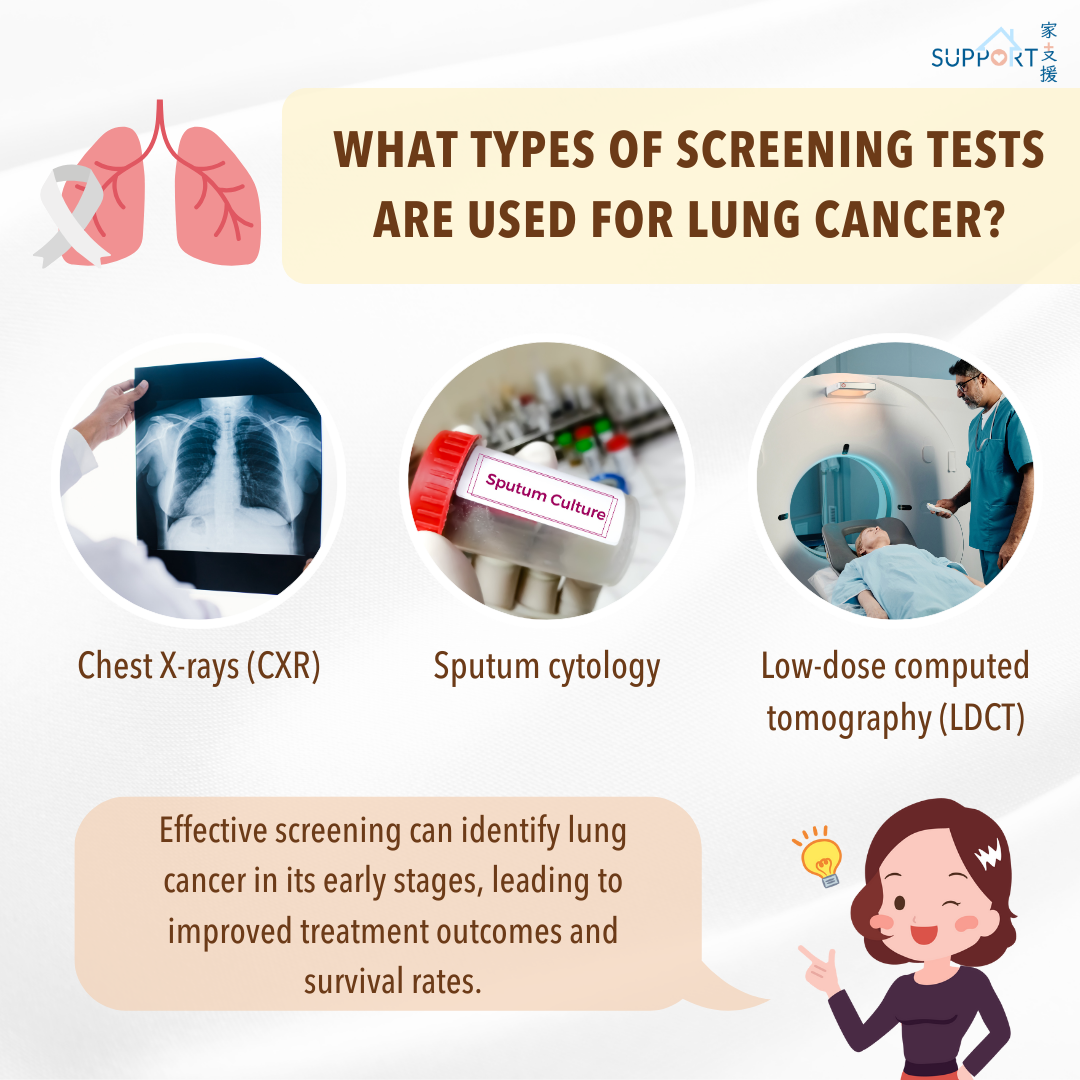
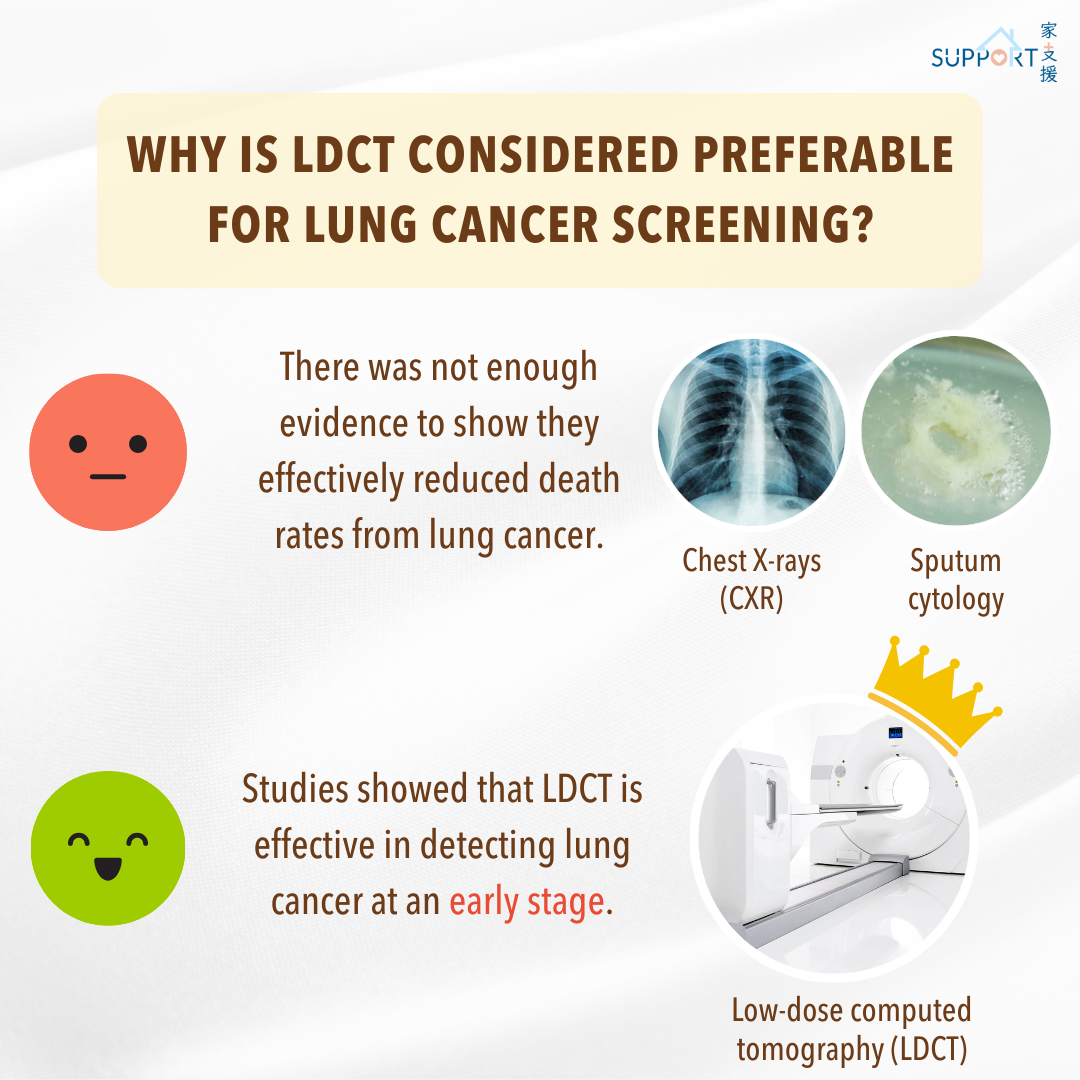
Since local guidelines haven't been fully established, individuals with a heavy smoking history should consult their doctors about the potential benefits and risks of LDCT screening. This includes understanding false-positive results and any follow-up tests that might be needed. It’s important to make an informed decision that is right for you. Please note that screening for lung cancer using CXR or sputum tests is not recommended.