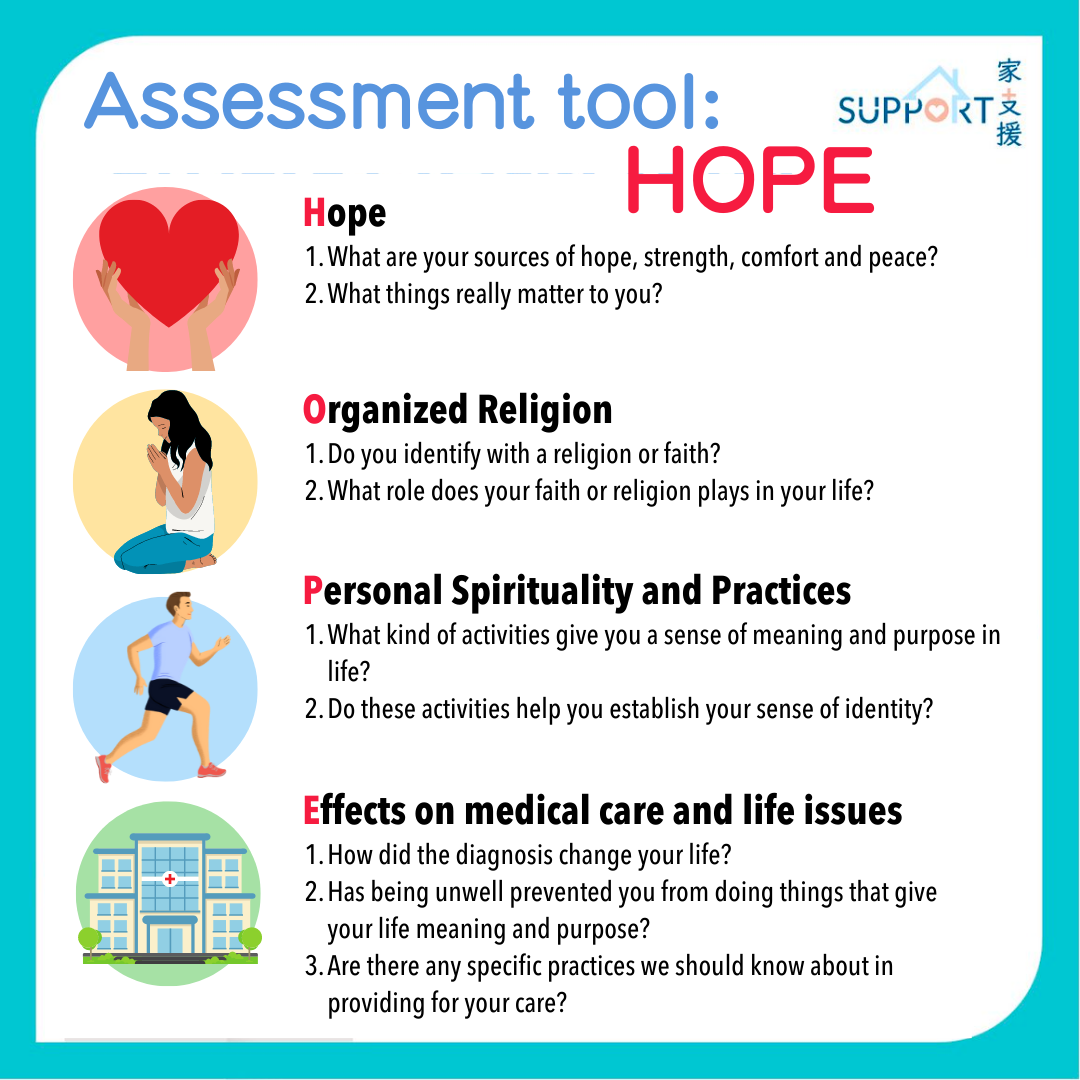
Spiritual support
Every family is unique in their spirituality, religion, culture, beliefs and values. Whatever one wishes for the patient’s care, consulting a healthcare team is always a solution. Being aware of different needs, health professionals should be able to help find solutions. Referrals to spiritual care workers can also be offered.
Spiritual care workers are trained professionals who help people work through their feelings spiritually. They are key members of the palliative care team. They can help arrange visits from religious figures such as ministers, priests, rabbis and imams, while educating and supporting others in caring roles by providing culturally sensitive spiritual care. If the patient is religious, possible interventions could include:
- Visits from, or referrals to chaplains, pastoral care workers or traditional healers
- Spiritual and/or religious counselling
- Taking part in religious services.
- Speaking to religious figures
- Guidance and professional opinion from a psychologist or counsellor
If the patient is not religious, possible spiritual interventions might include:
- Reviewing one’s life
- Joining support groups
- Listening to music
- Drawing
- Going outdoors
- Enjoying other leisure activities
- Seeking the opinion of a psychologist or counsellor
Culture support
Cultural needs differ among people with different backgrounds and education levels. If certain cultural needs are to be fulfilled, it is important to let the palliative care team know. Cultural practices may encompass aspects such as the diet, personal hygiene, clothing, along with special holidays and celebrations.
It is recommended that a professional interpreter be requested regarding important information, if the patient or their family has difficulty understanding English, Mandarin or Cantonese.