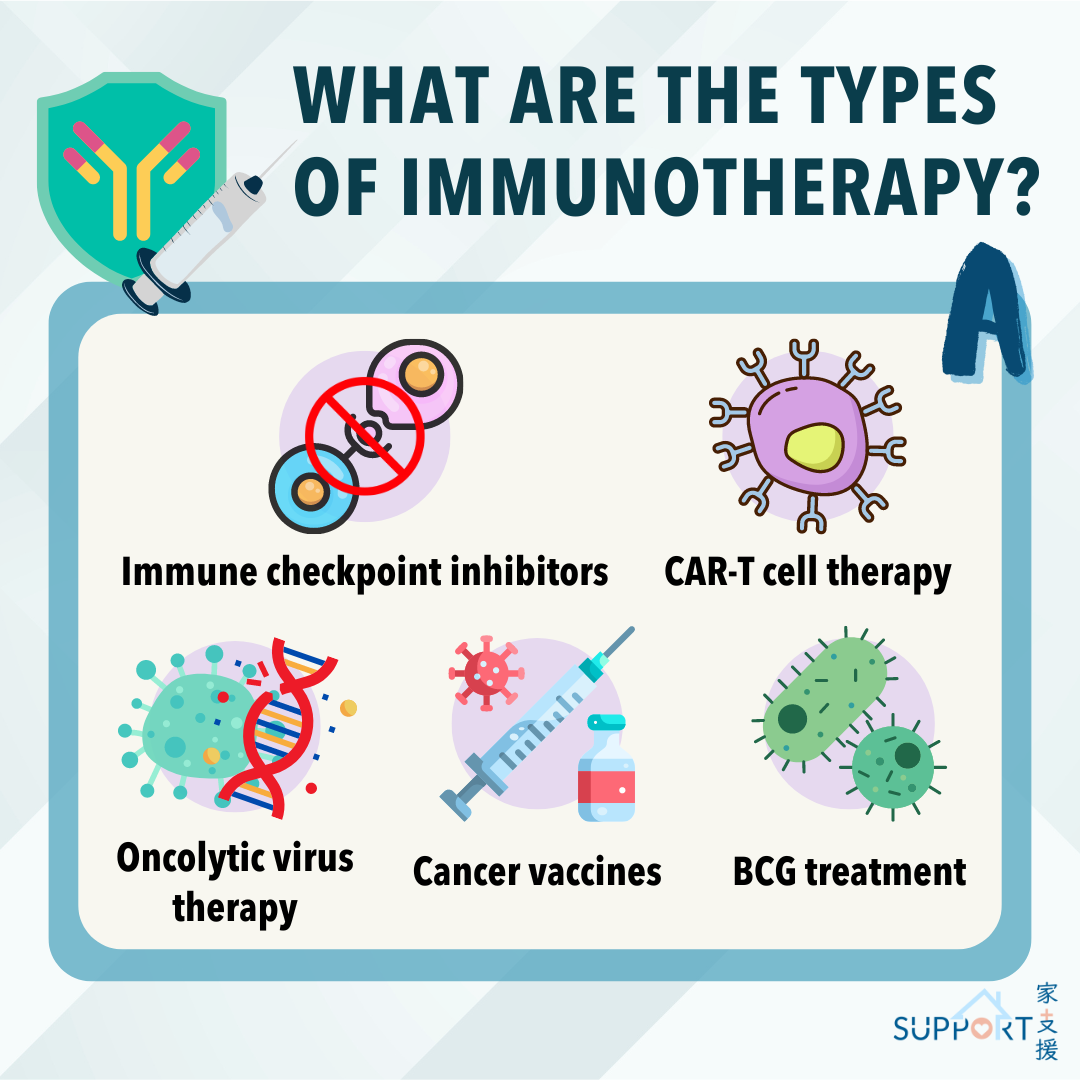
There are mainly five types of immunotherapy:
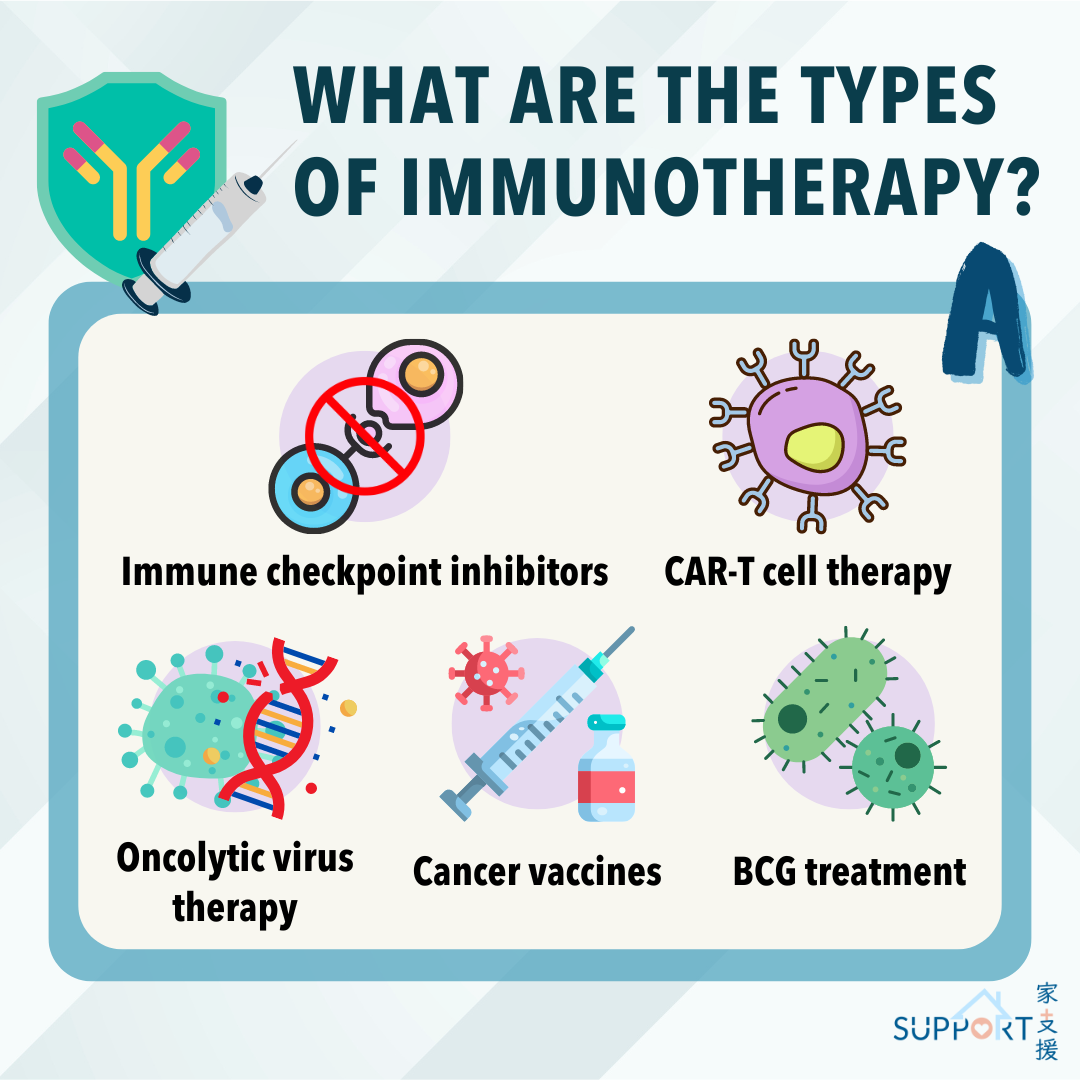
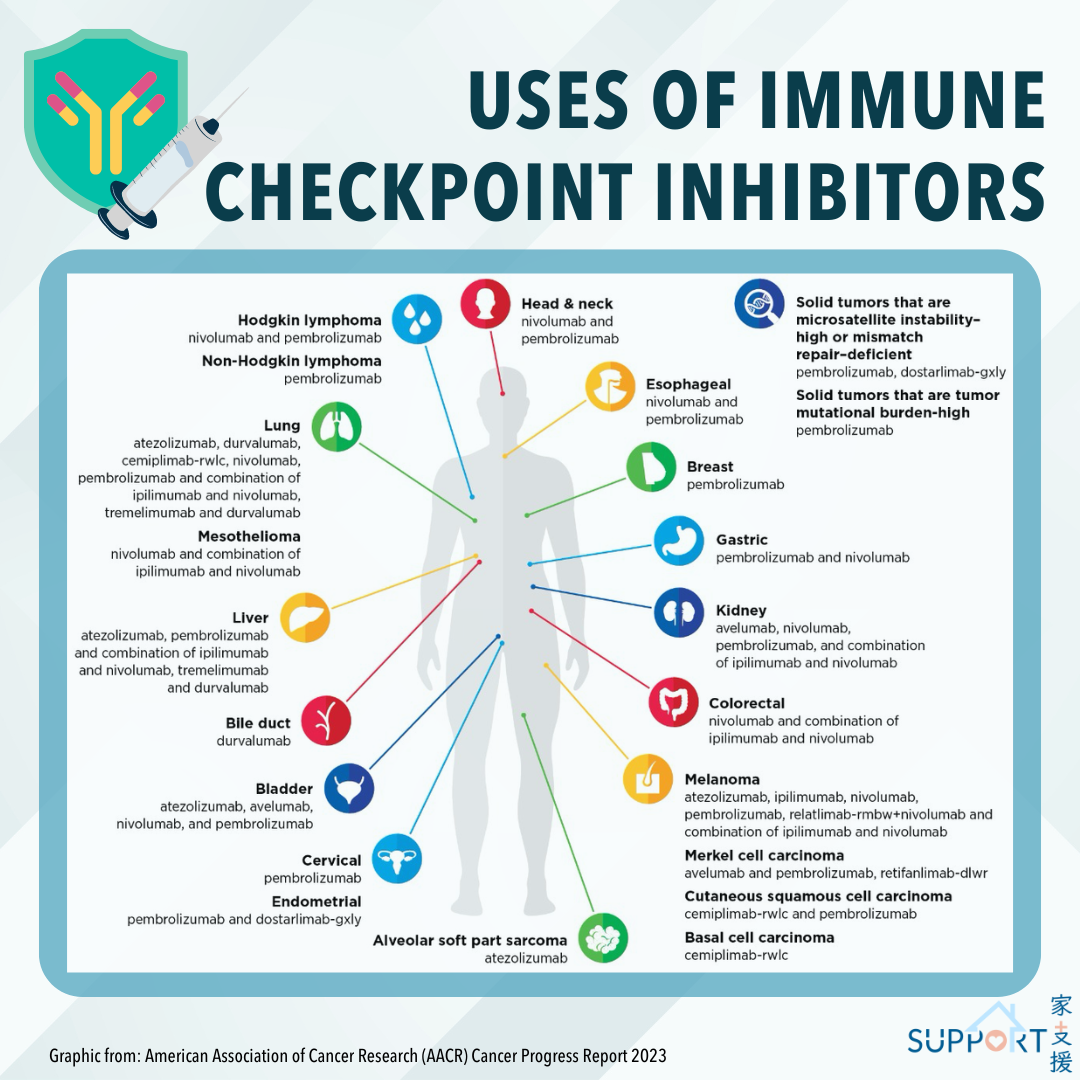
1. Immune checkpoint inhibitors
Immune checkpoint inhibitors are the most common type of immunotherapy. When certain proteins on the surface of immune cells (T cells, for example) bind to the proteins on cancer cells, an “off” signal is triggered, thus blocking the attack of T cells. This on/off switch is called “immune checkpoint”.
Commonly used immune checkpoint inhibitors can target proteins like CTLA-4 or PD-1 on immune cells or PD-L1 on the surface of cancer cells, avoiding the binding of the proteins on immune and cancer cells. This avoids an “off” signal from being sent, thus allowing the T cells to attack cancer cells.
2. CAR-T cell therapy
CAR-T cell therapy is currently mainly used for curing blood cancer. It involves collecting immune cells from the patient’s blood. The immune cells are then genetically altered in a lab so that they can recognize cancer cells. Finally, the modified cells are infused back into the patient’s body.
3. Oncolytic virus therapy
In recent years, research has been conducted to treat cancer, for example melanoma, with oncolytic viruses. Also known as virotherapy, oncolytic virus therapy involves modifying viruses with biotechnology to attack cancer cells. When cancer cells are infected with these lab-modified oncolytic viruses, the cancer cells burst and die, releasing cancer antigens that stimulate the immune system to attack other cancer cells.
4. BCG treatment
This is a type of immunotherapy commonly used for treating early-stage bladder cancer. After a patient undergoes endoscopic surgery, the doctor infuses a solution containing the BCG bacteria into the bladder through a catheter. The treatment typically lasts for one year and is aimed at reducing the risk of cancer recurrence.
5. Cancer vaccines
Similar to other viral vaccines, cancer vaccines, which are made up of proteins found on the surface of cancer cells (also known as "cancer antigens"), are injected into the patient’s body. This trains the immune system to recognize and attack the cancer cells associated with such antigens.